Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question was
You can check out last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer questions from one of my clients Julie as part of my 1:1 consulting and advocacy service! Julie’s mother is in the ICU for Pneumonia and she’s asking if the ICU team notice her mum’s growing abdominal girth.
My Mom is in the ICU for Pneumonia. Will an Increase in Intra-Abdominal Pressure Make My Mom More Critically Ill?
“You can also check out previous 1:1 consulting and advocacy sessions with me and Julie here.”
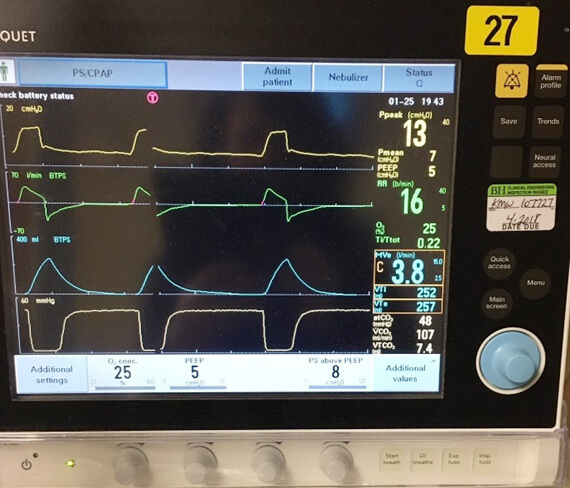
Patrik: Okay, good, good. Okay, now I’m looking at the monitor. Okay, yes. I can see her blood pressure is very low. As far as I can see-
Art: It has come up since I sent the picture. Right now, it’s about 111 over 66 with an 81 mean arterial pressure.
Patrik: Right. So that’s with the Norepinephrine going?
Art: I think so, yes.
Patrik: Okay, okay. The person that I see in the picture is the nurse?
Art: Yes.
Patrik: The reason I’m asking is why is he wearing a gown? Is Julie’s mom infectious? Do you wear a gown as well?
Art: Yes.
Patrik: Do you know why you’re wearing a gown? Have they given you a reason?
Art: I don’t know.
Patrik: Okay.
Recommended:
Art: She came in with pneumonia and a UTI. I guess the bacteria they identified as a highly-infectious bacteria.
Patrik: Most likely.
Art: It was not MRSA. It was something else.
Patrik: Okay. All right. And on day one they asked you to wear a gown?
Art: Since day two or three.
Patrik: Okay, okay.
Art: It wasn’t on day one.
Patrik: Sure, sure. Okay, okay. Right. That section where you can see the blood pressure on the monitor, okay? On the picture that you sent, I can’t see what’s on the left now because he’s brought up another screen on the picture. Because I’m wondering, is that blood pressure an arterial blood pressure or is it from a blood pressure cuff on an arm? Do you know the difference?
Art: Oh, I understand what you’re saying. There is a cuff on her arm that works automatically. It’s on her left forearm.
Patrik: Mm-hmm. Can you send me another picture of the monitor when there’s nobody in the screen? Because I’m just trying to find out if she does have an arterial line or not.
Art: Yep, hold on. One second.
Patrik: Thank you.
Art: Okay, that’s on its way.
Patrik: Thank you. Were you in the meeting yesterday yourself? Were you present? Were you part of-
Art: I was in the meeting. I was here today.
Patrik: Okay, okay. Because I am wondering, you mentioned that she is full code, which is good. But was that ever in question yesterday or today? That she may not be full code?
Art: No. She’s been a full code since arrival.
Patrik: Right. And that was never in question as far as you’re aware?
Art: No.
Patrik: Okay. Good, good. Because as soon as they start questioning it, you need to let me know. You need to let me know immediately. If they start questioning full code you will need to let me know, so we put a stop to that.
Art: Define, “Questioning.”
Recommended:
Patrik: Say that again?
Art: Define, “Questioning.”
Patrik: Yeah, okay.
Art: What do you mean by that?
Patrik: So, when it comes what I refer to perceived end of life situations, okay. I argue Julie’s mom is in a perceived end of life situation. Okay, it’s a perception, it’s not necessarily reality, okay. A real end of life situation is when people are dying and there’s nothing you can do, okay. So, at this point in time, yes, Julie’s mom is critical, but she’s alive. Okay, and they’re treating her. So that, in my mind, is a perceived end of life situation but it’s not real. So, in those situations, many times, the ICU wants to push towards end of life and wants to push towards DNR. You know what I mean by DNR?
Art: Yes.
Patrik: Right, right. And it’s also the first step to move patients towards withdrawal of treatment quickly. Right, the minute they bring up DNR, it’s a sign that they want to move towards withdrawal of treatment once the DNR has been signed. I’ve seen it over and over again. The minute DNR is mentioned.
Art: Oh, it has definitely been mentioned.
Patrik: Okay, but you can 100% say she is not DNR at the moment? You feel confident about that?
Art: Oh, 110%.
Patrik: Okay, yeah. That’s the main thing. The main thing is that she’s not DNR. That’s the main thing.
Art: Yep, absolutely.
Patrik: Did you send me another picture? I haven’t received it.
Art: I did.
Patrik: Okay, just give me one sec.
Art: Okay.
Recommended:
Patrik: No, haven’t received it, no.
Art: Have you received it yet?
Patrik: No, no. Haven’t, haven’t.
Art: Hold on one sec, let me see.
Patrik: Okay.
Art: Did you want to talk to the nurse?
Patrik: Absolutely, if he’s available, absolutely.
Art: Okay. Are you on speaker phone? I’ve been kind of having a little hard time hearing you.
Patrik: You have a hard time hearing me? Yes, I am on speaker phone, but I also wear a headset.
Art: Okay.
Patrik: I can take off the headset and I’ll get it. Just, let me know, can you hear me better now? Is this better?
Art: Yes.
Patrik: Okay, all right. I’ve taken off speaker, I’ve taken off my headset. Okay, that’s all right.
Art: Okay, yeah. He is. Are you ready?
Patrik: Yes, I’m ready.
Art: Okay, here’s Mel.
Mel: Hey there, how you doing?
Recommended:
Patrik: Very well, thank you. How are you?
Mel: Well, not too bad. You know, just another night in the ICU.
Patrik: Absolutely, you’re doing a night shift?
Mel: Yeah, yeah. I work seven-seven.
Patrik: Oh, my goodness, that’s a long shift. Look, Mel, I’m family friend and I’m an Intensive Care nurse by background myself, I’ve done the seven to seven days and nights and I still do them. So, I guess, the family’s pretty confused in terms of what’s happening, what’s going on. I would really appreciate if you can sort of give me a bit of a run down, if you can, so I can sort of refer it back to the family and explain to them what they’re dealing with. I know the pneumonia, I know the inotropes, I know the intubation on Tuesday. I know all of that.
Mel: Okay, so you’re more wondering about the GI stuff?
Patrik: Yes, the GI stuff, I would be imaging lactate might be going up, I don’t know.
Mel: So, I mean, basically where we’re at this point, they initially thought that there was a possibility that she may have puffed. They found after everything that she had a problem in her abdomen. They thought she may have puffed.
Patrik: Right.
Mel: The good thing, they’re still not completely sure.
Patrik: Right.
Mel: They’ve done two CAT scans, and of the two CAT scans, the first one, it showed quite a bit of error. The one they did this morning if you give me a second, I can pull up the actual notes. But it shows a decrease in error the abdomen from yesterday to today. So, the other thing is we’ve given her a total of two gallons of Go Lightly with basically no response. They had a very, very small smear today, but that was it. The original plan was to give her to Go Lightly and then do a colonoscopy. But because the Go Lightly didn’t work, they don’t feel like the colonoscopy is going to be able to tell them much. The impression on the CT scan today basically said, “Decreased bowel perfusion, mild bowel loss again is seen at the area…and decrease bowel motility.” So, they did see a decrease. It doesn’t really specify how much of a decrease.
Recommended:
Patrik: Sure, sure.
Mel: So, there’s still, GI at this point is still not exactly sure what’s going on.
Patrik: Sure, sure.
Mel: The original CT scan they initially saw a perforation, and they didn’t see a perforation but, as you know, that doesn’t necessarily mean that there’s not one. One of the biggest things right now is trying to understand why we’ve given her two gallons of Go Lightly and nothing has come out. So, I can tell you that last night when I assessed her, her abdomen was absolutely just rock hard. And it’s still pretty firm, but definitely softer than last night.
Patrik: Okay.
Mel: So, I mean, as far as the GI goes unfortunately that’s not that’s not what we know at this point. Her white count has gone way up, her red count went from 20 yesterday up to 40 today.
Patrik: Right, okay, I see, I see.
Mel: And so, they grew blood cultures today to see if she’s going septic. I mean her lactate went up a little bit but only 2.1.
Patrik: Okay, okay.
Mel: So, but she is pretty down. What I got in report was her fever had gone down to 102.1. She’s down to about 100.1 right now. But I mean I also wonder if, I’m assuming she’s shunting because her hands and her extremities are extremely cold.
Patrik: I see.
Mel: She’s got good circulation, but her peripheries are just really cold. So, her trunk is warmer. So, I mean she is febrile.
Patrik: Yeah. So, she might well be septic. She might well me septic. Sounds like she might be.
Recommended:
Mel: They don’t know for sure, but, I mean, it’s certainly possible. She could have an issue with her bowel. But I think that they’re leaning more towards assuming she’s probably puffed.
Patrik: Right, right.
Mel: Obviously, I can’t diagnose that.
Patrik: But it’s possible. Has a surgical consult been made? Is a surgeon-
Mel: Yeah, GI is following her. What I got in the report, and I’ve only been on for a couple of hours and obviously I’ve been in the room, so I haven’t really had a chance to look yet, sit down with all the notes yet. What I think the report was GI is feeling at this point like they can treat.
Patrik: I see.
Mel: I wasn’t here with her when GI came in, and I haven’t accessed those notes yet. But like I said, what I got in the report was they feel like they can treat, so.
Patrik: I see. And is she on vasopressors? Is she on-
Mel: She is on Neofrin. I’ve got her right now, she’s at 13.
Patrik: Right.
Mel: She’s on, right now she’s on 13 of Neofrin.
Patrik: And that’s my-
Mel: No, no, no, I’m sorry. I lied. I said 13. She’s on, I’m looking at the wrong pump, she’s on 80 of Neofrin. They had her up to 200. They had her max earlier today, she’s at 80 right now. So, and our orders at this point are, if we have to back up over 100 of Neofrin, they want us to start Vasopressin instead of continuing to go up on Neofrin.
Patrik: Sure. And when you’re saying 80, that’s micrograms per minute or what?
Mel: Correct.
Patrik: Right, okay, okay, okay. Kidneys, did you say earlier, kidneys are working or?
Mel: Kidney function, hold on, I looked at it, let me pull up the lab report.
Patrik: Thank you, thank you.
Mel: Yeah, her kidneys are functioning. I believe she had 1,500 out today.
Patrik: Right, that’s good.
Recommended:
Mel: And her BI is a little elevated, 44 on her pre-med and 0.44.
Patrik: Right.
Mel: But she has, both scans that I’ve done, I’ve got a report on her that she’s done a really good, solid urine output, so.
Patrik: Yeah, no, that’s right. Look, Mel, I, and she’s sedated with, is she sedated or is she in a natural coma?
Mel: Yeah, no. We’ve got her on 75 Propofol, 30 of Fentanyl and 20.6, hold on. 1.2 Precedex. Okay, so 1.2 Precedex.
Patrik: Precedex as well, okay. And the infection and the pneumonia has not been cleared yet, just what you mentioned. And, there is no way at the moment she would come off ventilation. I would imagine she’s-
Mel: No, no.
Patrik: She’s not breathing.
Mel: She wouldn’t tolerate. Yeah, no, she wouldn’t tolerate coming off the vent right now.
Patrik: Right. Hey, Mel, I really appreciate your time, I really do. And I think that’s enough information for me to put things in perceptive for the family.
Mel: Okay.
Patrik: Do you think there was anything else that sort of?
Mel: No, those are the big ones.
Patrik: Yeah, they’re the big ones. There’re the big ones.
Recommended:
Mel: The other thing that’s still kind of pending is waiting for the blood cultures to come back to see if she’s septic or not.
Patrik: Yeah, and I guess she’s probably way too unstable with all the vasopressors to go for surgery. I mean she wouldn’t go for surgery on Monday.
Mel: I guess is, yeah, GI wouldn’t clear their side as far as surgery at this point. They would want to get her down off the Vasopressors before they would actually take her for surgery.
Patrik: Obviously they’re giving antibiotics, I would imagine?
Mel: Yeah, we’ve got her on Fluconazole and Meropenem
Patrik: Meropenem.
Mel: There’s one other. Just let me get the report up.
Patrik: Flagyl?
Mel: What’s that?
Patrik: Flagyl or Metronidazole?
Mel: It might be Flagyl. Fluconazole. I think you’re right, I think it is Flagyl.
Patrik: Metronidazole is only Flagyl.
Mel: Yeah, yeah, yeah, Metronidazole, Flagyl and they started on the Meropenem.
Patrik: On this arm. Okay. And she’s not bleeding, there’s no haemoglobin drop or any of that?
Mel: No, no. I mean, her blood counts are good. I think her haematocrit was, I can pull it up. Her haematocrit was 41.
Patrik: It’s all right.
Mel: Her haemoglobin was 14 or, her haemoglobin was 15.5 and her haematocrit was 46.5.
Patrik: Yeah, that’s awesome. Hey, Mel, I really appreciate your time to take out of your day. I know you’re busy, yeah. Thank you so much, I really appreciate it, and have a good shift, mate.
Recommended:
Mel: All right. Appreciate it. You have a good night.
Patrik: You have a good night. Bye-bye.
Mel: Yep, you bet.
Art: Hi Patrik.
Patrik: Hi Art. So, that was very, very helpful. Do you want me to explain it to you, do you want to get other family members while I’m explaining, what do you want me to do?
Art: I followed along for most of it. But, I mean, yes, please give me your interpretation.
Patrik: So, I’ll tell you what my interpretation is.
Art: You know what, I’m going to walk out to the waiting room.
Patrik: Yeah, that sort of thing, whatever.
Art: And this way you can explain it to the family.
Patrik: Exactly, that’s what I thought. Do you want me to call you back in a minute or?
Recommended:
Art: Yeah, actually if you can, can call me back on the number I gave you?
Patrik: Yes, on the number-
Art: I think this phone’s at like, 3%.
Patrik: I’ll call you back now? Straight away? Thanks.
Art: Yeah. That’s fine.
Patrik: Thanks, bye.
The 1:1 consulting session will continue in next week’s episode.
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!







