Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED“ and in last week’s episode I answered another question from our readers and the question was
You can check out last week’s question by clicking on the link here.
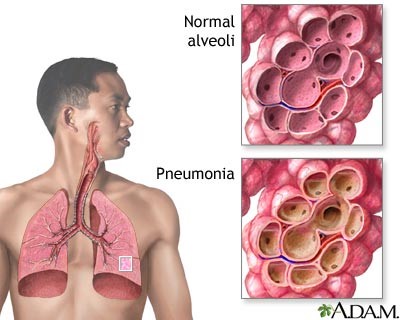
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer questions from one of my clients Julie as part of my 1:1 consulting and advocacy service! Julie ’s mother is in the ICU for Community Acquired Pneumonia and Julie is asking if the infection in her blood(sepsis) could be a reason why the ICU team wants to limit treatment options and “pull the plug”?
My Mom is in the ICU for Community Acquired Pneumonia. Will The Infection in Her Blood Lessen Her Chance of Living?
Patrik: We believe that nurses are real advocates and don’t have … like a lot of the doctors have interests that go way beyond treating a patient. They have interests that … you know if you’ve done a little bit of research, they have interests in medical research, they have interest in getting money through medical research, but don’t necessarily have the interest in treating patients appropriately. Whereas as we, as nurses, we are genuine advocates. And again, I don’t know how much research you’ve done. You can listen to some interviews on our website, on our podcast. Where we interviewed some of our clients, how we help them to get outcomes. Because we don’t really care what the doctors think. We are advocates. Whereas, if you have another doctor coming in, they’re often protecting each other.
Jane: That sounds like what Julie needs. So, let’s get down to brass tacks, and first, what’s your name?
Patrik: Patrik.
Jane: Patrik?
Patrik: Yeah.
Jane: Okay. And then so what do we have to do to make this phone call happen?
Patrik: Yeah, I can tell you what you need to do. So, you would need to engage my service. That’s number one. And then you would need to set up a phone call with the doctor, right? Whatever time, I can make myself available. Right? You-
Jane: Okay, and what does the service cost?
Patrik: Pardon.
Jane: What does the service cost? What are we- ?
Recommended:
Patrik: Yeah. I’ll give you some options. I’ll give you some options after. I’ve got several options. I have a two-week phone option that gives you two weeks unlimited 24-hour access to me. It includes talking to doctors and nurses. It includes talking to you, of course, whatever is involved, right? It’s 24 hours unlimited phone service for two weeks.
I have a seven-day option. The same rules apply, seven days, 24 hours unlimited access to me. It includes talking to you, of course, talking to the doctors and nurses. If you have any meetings, I will be there over the phone.
I have a four-day option, and I have an hour option. The hour option can be credited towards the four-day, the seven-day, or the 14-day option.
Also, with the four-day, the seven-day, or the 14-day option, you are in control when you want to use it. So, you don’t need to use it four days in a row or seven days in a row or 14 days in a row. You are in control when you want to use it. You can spread it out. And I have a-
Jane: You need to use it.
Patrik: Right, and I have an online-
Jane: How many hours per day?
Patrik: Whatever you need, whatever you need.
Jane: Oh, okay.
Patrik: Right whenever you need. We try and work on our-
Jane: If we decide on which package we want then, how do we go about contracting with you?
Patrik: Yeah. So, the next step would be, I will send you an email with the consulting options, and you just click on the link and you can pay, make payment there with a credit card or via PayPal, either or.
Jane: Okay.
Julie: Okay. And then so do you have, with your business and your credentialing, do you have a lot of say? Like when you talked to a doctor, is it … How do you …? credited advice?
Patrik: Yeah, yeah. I tell you how I normally operate. Okay. And I’ll be guided by you, because you can read the situation or you can read the dynamics with the doctors better than I can at the moment, right? I tell you how I normally come in.
Recommended:
Patrik: So, we take a non-threatening approach to begin with. And if we think we’re not getting anywhere with the friendly approach, we would change tact, okay? But in the beginning, let’s try a friendly approach.
Julie: Yes, this is the first … I just feel so good about this. Okay. Thank you so much. I’m sorry, I’m just getting a little bit emotional.
Patrik: Right. Let’s take a friendly approach in the beginning. Let’s find out what’s exactly happening. Let’s remind them, friendly, that they have a duty of care for you and for your mother. Right? And if that doesn’t work, we’ll change tact.
Julie: Okay.
Jane: Okay. So, we just need to … so after we obtain the services, we get your phone number directly, and then we get a hold of him tomorrow, and he can call you or you can call him? Or can we do it tonight? Can-
Patrik: We can do it tonight. If you can get hold of the doctor tonight, we can do it tonight. Really up to you.
Mike: Do you have any way to track down the doctor on the phone tonight? ‘Cause he’s kinda got to voluntarily-
Patrik: I tell you what the best way would be to go about it. It would be good if I can get information to begin with the bedside nurse or with the nurse in charge or with a junior doctor there. And the more information I have before I talk to the senior doctor, the better it is. Does that make sense?
Recommended:
Patrik: Are you in hospital at the moment?
Julie: Yes. Yeah.
Jane: Yes, we are.
Patrik: Right. Okay. Could you … after you’ve engaged my service, could you pull out your cell phone and get the nurse, the bedside nurse on the phone? Do you think you can do that?
Jane: If they’ll legally take the phone. Yes, I can try.
Patrik: Yeah, yeah. Yeah, yeah. One important thing in this situation is always to not over-complicate. It’s really important not to over-complicate. You know, you might just go to the bedside casually, and you might say, “Hey, here is my auntie’s friend on the phone. Can he ask some questions?” You know, make it casual, nonthreatening to begin with, and don’t over-complicate. Get somebody on the phone, so we can get information.
Julie: Okay. So, do we call you back then at this same number?
Patrik: Yes, same number. You will get me on the number you called. So, what I would like to do really is, I would email you the consulting options, and then you can select from there. And then as soon as you’ve gone through the payment options, we can get on the phone straightaway.
Jane: You have the number on your phone?
Julie: Yeah.
Jane: So, give him your email.
Patrik: Okay, all right. I’ll send you that email in the next couple of minutes, and then we’ll get on the phone with them.
Julie: Okay. Thank you so much.
Patrik: Thank you. Talk soon. Bye-bye.
Julie: Bye-bye.
Patrik: Okay?
Julie: Hello Patrik, I’m hearing that they just need to have the code.
Patrik: A code? You mean the nurse needs the code?
Julie: Yes, and the code is 7****.
Patrik: Hang on, hang on, I need to grab a pen and paper, hang on. 7**…
Julie: 4*.
Patrik: Yep. That’s it?
Julie: Yep.
Patrik: 7****. So, what are you going to do? How do you go about it? Will you go to the bedside and pull out your cell phone? How do you go about it?
Julie: Yes.
Patrik: Okay, okay and are-
Julie: Yes, I’m doing it and he’s in the room.
Patrik: Okay and just tell me. Your mother’s been ventilated since Tuesday? At the moment she is on Precedex?
Julie: Yes.
Patrik: Right. Do you know whether she’s on any inotropes or vasopressors? Do you know what I mean by that?
Julie: No.
Patrik: No. That’s okay. Do you know whether she’s on, have you heard of Adrenaline?
Julie: Here, let me let you talk to my fiancé because he will know all that.
Recommended:
Patrik: Sure, sure.
Art: Hello.
Patrik: Hey. Do you know? Are you Julie’s mom?
Art: Yes.
Patrik: Right. And so, what was your name?
Art: Art.
Patrik: Sorry?
Art: Art.
Patrik: Oh, okay. Do you know if Julie’s mom is on inotropes or vasopressors such as Adrenaline? Do you know?
Art: She’s on Phenylephrine.
Patrik: Okay. So she is. Phenylephrine is an inotrope. Okay. Good. That’s good information. Anything else, can you see? So, you can see Phenylephrine. Can you see Epinephrine or Norepinephrine?
Art: No.
Patrik: Okay. Can you see Dobutamine?
Art: No.
Patrik: Okay. Can you see how much Phenylephrine she’s on? Can you see a number?
Art: 80 micrograms a minute.
Patrik: 80 micrograms. Okay. Okay. Also, what would be valuable to know, do you know whether Julie’s mom has any other significant pre-medical history besides what we talked about before?
Art: Has any what history?
Patrik: Any other significant pre-medical history. For example, as far as you’re aware, her heart is fine?
Art: Yes.
Recommended:
Patrik: Okay. Her kidneys are fine?
Art: Yes.
Patrik: And the liver is fine as well as far as you’re aware?
Art: Yes.
Patrik: Okay. So, we’re really talking about single organ failure. Which are the lungs. She’s not breathing at the moment. And potentially the gut is failing but we’ll find out what’s exactly happening there. Do you know if she’s still on any antibiotics?
Art: They started her on another antibiotic today.
Patrik: Mm-hmm.
Art: I don’t know if it’s still. I think that might be it, Fluconazole.
Patrik: Okay, okay. Okay, Fluconazole. Okay, Fluconazole is an anti-fungal. But that’s okay. That’s okay.
Art: Oh. Okay.
Patrik: That’s all right. That’s all right. It’s no big deal. Could you also at some point, it doesn’t have to be right now. Do you think you could send me a picture of the ventilator and the monitor?
Art: Oh. Yeah.
Patrik: That would be very helpful. But now that I’m-
Art: Do I do that to that number that we text messaged?
Patrik: Yes, please. Yeah. Or you can email it.
Recommended:
Art: Hold on one second. I can do it really quick.
Patrik: Or you can email it. Whatever is easiest.
Art: Hold on one second.
Patrik: Yeah.
Art: Hold on one second, I’ll text it to you.
Patrik: Yeah.
Art: Okay its on its way.
Patrik: Okay. Just give me one second.
Art: Hey, Patrik, I’m going to give you my phone number as well.
Patrik: Okay.
Art: Because the battery on this phone is a little low.
Patrik: Okay, can you text me your phone number please?
Art: Yeah. I’ll do that right now. Hold on. Okay. It’s on its way.
Patrik: Okay. Thank you. I’ll just wait. There is no other equipment around the bed space? There is no dialysis machine, it’s just the ventilator You’ve noted the-
Art: It’s just the ventilator and IV medications.
Patrik: Okay. I’m just looking at the ventilator now. She’s on a fair amount of sedation there. So, she’s not breathing by herself. She’s getting everything from the machine. But that’s okay. Now I have enough information to talk to the nurse. When I talk to the nurse, how are you going to introduce me to her? Who am I?
Art: As a friend of the family.
Recommended:
Patrik: Okay, yeah. That’s great. I just need to know, I can say I’m a friend, I’m Patrik, I’m a friend of the family, I’ve worked in Intensive Care. And the way I approach it is, look, the family is very unclear of what’s exactly happening, can I get, you know, explain the situation to me. That’s how I will approach it. Very, very friendly, non-threatening. And the nurse who’s on duty at the moment, is she friendly, is she not friendly, what do you think?
Art: He seems friendly.
Patrik: Oh, he’s a guy? Male nurse?
Art: Yes.
Patrik: Oh, good. Good. Probably better. Yeah, I’m ready whenever. And what’s the guy’s name? Do you know?
Art: It’s Mel.
Patrik: Mel. Okay. I’m ready whenever Mel is ready to talk to me.
Art: Okay. As of right now, I’m looking at the monitor. Her mean arterial pressure is low again.
Patrik: Can you send me-
Art: It’s at 55.
Patrik: Can you send me a picture of the monitor as well?
Art: Yep.
Patrik: Thank you.
Art: Going to be just a second.
Patrik: Thanks. Thank you.
Art: Okay, that’s on its way.
Patrik: Thank you.
Art: Oh. They have another medication ready to go for her blood pressure too the Norepinephrine that you mentioned before.
Recommended:
- YOU DON’T KNOW WHAT YOU DON’T KNOW WHEN YOUR LOVED ONE IS CRITICALLY ILL IN INTENSIVE CARE! (PART 1)
- YOU DON’T KNOW WHAT YOU DON’T KNOW WHEN YOUR LOVED ONE IS CRITICALLY ILL IN INTENSIVE CARE! (PART 2)
Patrik: Okay, okay, okay. Right, okay. Are you aware of arterial blood gases?
Art: I’m sorry?
Patrik: Have you heard of arterial blood gases?
Art: Yes.
Patrik: Has she-
Art: That was kind of what lead to her being intubated because they did an arterial blood gas test and she was acidic.
Patrik: I see, I see.
Art: And it was down about 7.23ish.
Patrik: Right, okay.
Art: can’t remember the exact number off the top of my head.
Patrik: Sure. No, that’s fine, that’s fine. Okay. And, have you heard of lactate?
Art: Yes.
Patrik: And do you know what the lactate is at the moment? Got any idea?
Art: I know it was tested this morning and that was at 2.1.
Patrik: Yeah, okay. Because there’s a very high chance that if they’re starting Norepinephrine now that the lactate might be going up, but I will ask her that.
Art: Okay.
Patrik: Or him. Sorry, him. I will ask him that, once I get him on the phone. Do you know if there is a DNR in place? Do you know what I mean by DNR?
Art: As of right now she is a full code.
Recommended:
Patrik: Okay, good, good. Okay, now I’m looking at the monitor. Okay, yes. I can see her blood pressure is very low. As far as I can see-
Art: It has come up since I sent the picture. Right now, it’s about 111 over 66 with an 81 mean arterial pressure.
Patrik: Right. So that’s with the Norepinephrine going?
Art: I think so, yes.
Patrik: Okay, okay. The person that I see in the picture is the nurse?
The 1:1 consulting session will continue in next week’s episode.
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!







