What is intubation?
Intubation,(Tracheal intubation) is the placement of a flexible plastic tube(Breathing Tube or Endotracheal Tube) into the trachea (windpipe), through the mouth or sometimes through the nose, to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill or anesthetized Patients to facilitate mechanical ventilation with Ventilators (Breathing Machines) of the lungs, and to prevent the possibility of aspiration or airway obstruction.
- Purpose
- What is done?
- What are the Risks?
Purpose
Tracheal intubation is indicated in a variety of situations when illness or a medical procedure prevents your oved one from maintaining a clear airway, breathing, and oxygenating the blood. In these circumstances, oxygen supplementation using a simple face mask, Non- Invasive Ventilation(NIV) or BIPAP is inadequate. This scenario may occur for a number of reasons, but can usually be narrowed down to
- the inability for your loved one to breath for him or herself
- Depressed level of consciousness
- if protective airway reflexes such as coughing and swallowing are diminished or absent
- decreased oxygen saturation(oxygen levels in blood) or hypoxaemia(lack of oxygen) through rib fractures, Pneumonia, respiratory failure
- airway obstruction through swelling, foreign bodies, smoke inhalation
- certain drugs(anaesthetic drugs or opioids)

What is done?
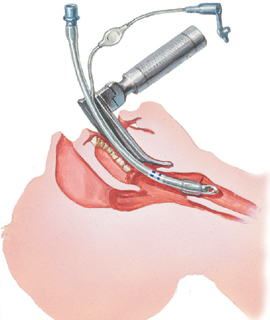
Because intubation is an invasive and extremely uncomfortable medical procedure, it is usually performed after administration of general anesthesia and a neuromuscular-blocking drug(muscle relaxants or paralysing agents). It can however be performed in an emergency without any anesthesia at all. Intubation is normally facilitated by using a conventional laryngoscope, flexible fiberoptic bronchoscope or video laryngoscope to identify the glottis the entry to the trachea(wind pipe), though other devices and techniques are available.
After the trachea has been intubated, a balloon cuff is typically inflated(to create a seal around the tube to protect the trachea) just above the far end of the tube to help secure the Breathing Tube or Endotracheal Tube, to prevent leakage of respiratory gases, and to protect the trachea from receiving undesirable material such as stomach content and stomach acid. The tube is then secured to the face or neck and connected to a breathing machine(Ventilators (Breathing Machines). A Chest X-ray is done to confirm the correct position of the Breathing Tube or Endotracheal Tube.
Normally, it is difficult for a Patient to tolerate a breathing tube and your loved is very likely getting sedative drugs(Propofol or Midazolam) and pain medication(Morphine or Fentanyl), in order to be able to let the ventilator do its work.
Whilst intubated, your loved one is unable to talk and it is important that if your loved one is awake to not stimulate them too much and talk to them in a calm and quiet manner. Because they can’t respond to other people’s talk it is very important to reassure your loved one. Usually the bedside nurse will explain everything that is done to your loved one and will also reassure your loved one.
Once your loved ones condition allows, the tube will be removed, this is called Extubation.

What are the risks and complications?
Most common complication associated with intubation are
- throat and lip laceration
- chipped, fractured or dislodged teeth
- irregular heartbeat
- high blood pressure(hypertension)
- elevated intracranial pressure
- bronchospasm
- laryngospasm(spasm in the windpipe)
- perforation of the trachea(windpipe) or esophagus
- pulmonary aspiration of gastric contents or other foreign bodies
- fracture or dislocation of the cervical spine
- decreased oxygen content
- elevated arterial carbon dioxide(CO2)
- vocal cord weakness
- Ventilator associated Pneumonia
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care procedures carry a degree of risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one and of course, if you have any questions or concerns, please ask the nurses and doctors in Intensive Care.
The information contained on this page is general in nature and therefore cannot reflect individual Patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
Related articles:
- How long can a breathing tube or an endotracheal tube can stay in?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Why does my loved one need a Tracheostomy in Intensive Care?
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- Be more selfish if your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 4 ways on how to be more persuasive if your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- How long does it take to wake up from a Traumatic brain injury or severe head injury
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


