Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED“ and in last week’s episode I answered another question from our readers and the question was
How Can I Have Power Over the Doctor’s Decision to Transfer My Dad from ICU to LTAC?
You can check out last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer questions from one of my clients Francia, as part of my 1:1 consulting and advocacy service! Francia’s dad is with a tracheostomy and is on a ventilator in ICU. Francia is positive that her dad can be weaned off the ventilator but the ICU team says otherwise.
I am Positive That My Dad Can Be Weaned Off the Ventilator, But The ICU Team Says He Can’t? Help!

Patrik: Sure. Okay. Any other medical issues? Does he have heart issues, kidney issues, or liver issues?
Francia: No. He has thalassemia. He received about a dozen blood transfusions in the hospital.
Patrik: Right.
Francia: That’s been going … Now, I don’t know. At home, his blood tests were good. No other medications beside morphine. He was on 30 milligrams. He was going on 15 at home. No medications though. And yeah, he’s on, Jevity at the hospital too regarding her nutrition, the PEG. So I don’t know if that’s contributing to what’s going on with his hemoglobin and everything else, but he does have thalassemia. He was diagnosed with the minor.
Patrik: Can you say that again? What was he diagnosed with?
Francia: Thalassemia.
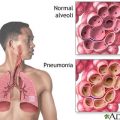
Patrik: Thalassemia. Oh, got it. Yeah, it is a blood disorder involving lower than normal amounts of an oxygen carrying protein. So he’s been getting red blood cells.
Francia: He’s been getting blood transfusions in the hospital. Before that, he never got one. His sister has it. His sister’s daughter has it. So it’s a genetic trait.
RECOMMENDED:
Patrik: Right. It’s a genetic trait. Okay.
Francia: He never got transfusions before either, and he’s got damn near a dozen in the hospital because it keeps going up and down, his hemoglobin from 6 to 9, but it’s stabilized now. They gave him iron, but that’s another thing. He’s had a bunch of fevers in the hospital. They put him on a bunch of runs of IV antibiotics. And the doctors are also saying now like they think he might not be able to wean off, but at the same time, he’s been so shot out and fatigued by all this. I don’t think they know.
Patrik: Absolutely.
Francia: Yeah.
Patrik: And he’s got a PEG feeding tube?
Francia: Yes.
Patrik: And he’s absorbing his feeds. There’s no issues with bowel movements as far as you’re aware.
Francia: It seems to be doing all right. He has a bed sore. It’s all right. It seems to be healing. So the Jevity seems to be absorbing well.
Patrik: Okay.
Francia: She seems to be assimilating it.
Patrik: Right. Francia are you the medical power of attorney for your mom?
Francia: Yeah, I’m his daughter, and I’m the POA.
Patrik: Great. Well, the bottom line is this, Francia. He can’t go anywhere really without your consent. Right? Especially since the health insurance is prepared to keep him where he is. Can you visit your dad or is everybody locked-
Recommended:
Francia: Yeah, I’ve been seeing him. No, I get exemption. I’ve been seeing him every day.
Patrik: Wow. That’s amazing. You’re one of the few people that can actually enter a hospital.
Francia: Yeah. I got an exemption.
Patrik: That’s great. That’s good. And if they were to send him to LTAC, have they given you an idea where that might be?
Francia: Yeah. Well, yeah, it would be at another hospital close by.
Patrik: Right.
Francia: Yeah. I have a list of different LTACs and SNFs to review, but-
Patrik: Right. How far away would that be?
Francia: Not far. It’s 25, 30 minutes.
Patrik: Okay. And can you visit there?
Francia: I don’t know because I had to make a special exemption, because currently, they don’t allow visitors, so I had to make an exemption. I hope I can make it with the other facility too. I don’t think they allow people right now.
Patrik: Right. Sure. Look. What do you see as your biggest challenge at the moment? Is it the pending transfer to LTAC? Would you say that’s your biggest challenge?
Francia: I’m not too worried about that. They’re pushing it, but patients’ rights … So an LTAC would be an acute hospital. The patients’ rights states that you don’t have to transfer … If a patient doesn’t consent to a transfer to another acute hospital, if then the hospital is providing the necessary care, then they could stay at that facility, as long as insurance covers it.
Patrik: Exactly.
Francia: So I’m not concerned. The thing is I don’t know why they’re pushing so hard for him to go to an LTAC or an SNF.
Patrik: They want-
Francia: Is it a monetary thing?
Suggested link:
Patrik: Oh yeah, definitely a monetary thing. It’s a bed management thing. Especially with COVID at the moment, they need hospital beds. They need ICU beds, all of that. So, Francia, how I can help generally speaking is just by talking with you to the doctors. I can set you up with clinical questions. I can certainly help you advocate to keep your dad in the right environment. That is certainly something that I do all the time, all day, every day if that is what you want. I always believe that hospitals, ICUs, they only tell families half of the story. And what I mean by that is they tell you what they think is relevant, but they’re not telling you half of the other things that are happening.
Patrik: When you and I get on a call with the doctors, I have a whole list of questions that I’m asking, and you will find that most of those questions will bring more things to light. They’re only telling you things that they think you (a) understand, and (b) helps them to have their needs met. And I’m looking at, okay, what else is going on? What else should you be knowing as the power of attorney?
Francia: Right. I understand. Right.
Recommended:
Patrik: Any talk about stopping treatment, any talk about DNR? Do you know what I mean with DNR?
Francia: What’s DNR?
Patrik: DNR stands for do not resuscitate. Sometimes when people are in a situation like that, the hospitals often ask, “Oh”-
Francia: No, I got that. Yeah. My dad said he would want to get resuscitated if it came down to that. He definitely wants to live.
Patrik: That’s great. That’s really good. Okay. So that’s where I can help you going forward. How often do you get updates from the doctors? Every day when you’re going there?
Francia: With these doctors, it’s a merry-go-round of doctors, so it’s eight-day interval. So every eight days, they switch up his doctor.
Patrik: Yeah.
Francia: Usually, every other day, the doctor will give me a call or I might catch him when I’m there with my dad.
Patrik: Yeah.
Francia: They gave me the same story because I believe it’s a conflict of interest if one doctor is to disagree with the others. So if there’s an opinion, they’ll keep it.
Patrik: Yeah, sure. Yeah.
Francia: Their consensus right now is they don’t think he’ll be able to, I guess to wean off, or if he does, to keep … What they’re saying is they want to send him to an SNF. They’re actually saying an SNF. He could go to an LTAC as well, but their reasoning for sending him to a SNF is, “Oh, it’s for rehab.” In your opinion, is that a bunch of selfish reasoning? Is it just a bunch of evil reasoning?
Recommended:
Patrik: Oh yeah. It’s crap. I’ll tell you why. So if your dad was getting regular physical therapy, the ICU would be the right place. They are telling you he needs to go to an LTAC because he would get physical therapy there. Yes, he will get that, but the problem is that he won’t be having an ICU nurse. He won’t be having ICU doctors. He won’t be having the same level of care. He won’t be having one-to-one or one-to-two nurse-to-patient ratio. In LTAC, it’s often one-to-five, sometimes one-to-10. So yes, he might get physical therapy, but every other aspect of care will be deteriorating.
Francia: Right. I’ve heard that. Yeah.
Patrik: I describe LTAC as a better version of a nursing home.
Francia: Yeah, it’s a better version of a skilled nursing facility. Right?
Patrik: Very much so, but it’s not ICU. That’s why I am so opposed to LTACs because from my experience and also from research and evidence-based practice, a patient on ventilator/tracheostomy needs an ICU nurse 24 hours a day, and they’re just not getting that in LTAC.
Francia: That’s right. And definitely not in a skilled nursing facility.
Patrik: Definitely not in skilled nursing facility, and definitely not in LTAC. So the risk of him going there is huge. The missing part at the moment is definitely that he is not getting enough physical therapy. That’s definitely a missing link, but you almost have to weigh up what’s more important? Is it the physical therapy? Is it the overall safety? It’s-
Francia: Yeah. And if I could go in and do physical therapy with him, and I’m willing to do that every day to move his legs, move his arms, maybe manipulate his back,
Patrik: Absolutely.
Francia: So other than that, I don’t see an actual reason, except business practices for the hospital.
Patrik: Yeah. Look up online reviews for LTACs. They’re usually pretty bad.
Recommended:
Francia: Yeah, they are. Yeah.
Patrik: They’re pretty bad. You already know what you’re signing up for. Francia, my time is limited, unfortunately. I believe we sent you the consulting and advocacy options in an email.
Francia: Yes. Yeah, I received those.
Patrik: If you wanted to continue the conversation, if you wanted me to talk to the doctors with you, we can do that.
Francia: Yes, Patrik. Yeah. I have no problem paying for your time in helping me. I definitely would appreciate you talking and speaking with the doctors and helping me with this.
Patrik: Yeah. There’s no issue there. You let me know how you want to proceed. I think we emailed you the consulting options and then go from there.
Francia: Okay. Excellent.
RECOMMENDED:
Patrik: Please note, I do work on a first come first serve basis. That’s all.
Francia: Okay. No, I understand.
Patrik: Any questions regarding those consulting options, please let me know.
Francia: Okay. Definitely. I’ll respond to your email. Okay?
Patrik: Great. All the best for now, Francia. Nice to talk to you.
Francia: Thank you. You too.
Patrik: Thank you. Bye. Bye. Bye.
The 1:1 consulting session will continue in next week’s episode.
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to Eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to you and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!