Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED“ and in last week’s episode I answered another question from our readers and the question was
The Medical Team Wants My Dad On A DNR (Do Not Resuscitate) Status. What Should We Do? Help!
You can check out last week’s question by clicking on the link here.
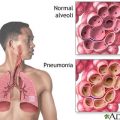
In this episode of “YOUR QUESTIONS ANSWERED” I want to answer a question from one of my clients Anna as part of my 1:1 consulting and advocacy service! Anna’s dad is in ICU due to pneumonia and sepsis. Anna is asking for advice about her dad’s treatment and prognosis.
My Dad is Admitted in ICU Due to Pneumonia and Sepsis. How Do We Move Forward with my Dad’s Care?

Dear Patrik,
I have found your website an invaluable help over the last 6 weeks that my Dad has been in Intensive Care here in the UK. My Dad was admitted to hospital for respiratory distress/double pneumonia and sepsis.
He was on the Respiratory Ward for initial 24 hours, and then transferred to ICU when his breathing deteriorated.
I decided to contact you as, like many families you work with. Dad’s condition is complex with many unknowns attached. I would very much welcome your help and expertise in terms of how we move forward with my Dad’s care re: prognosis and treatment options.
RECOMMENDED
To give you a background & history:
My Dad is 76. I would describe him as generally healthy. He really enjoys life and is a very kind and loving, decent, well educated person. He is a company director with two busy businesses.
I would describe him as very strong psychologically. He is a very even tempered, calm person.
He does have COPD (he smoked until 15 years ago, when he gave up successfully after years of us bullying him!!!) and developed Type 2 diabetes approximately 4 years ago, for which he takes Metformin.
He has never needed treatment for his COPD and, actually, rarely gets chest infections.
My Dad lives with my stepmom and my brother lives locally.
My sister and I both live 150 miles away but we are a very close family and are always in touch.
Sunday
My stepmom notices my Dad seems unusually quiet at breakfast. Says he is just thinking. He drives to visit my brother, who notices he has trouble parking the car. He comes into the house, is unsteady, then sits down and falls asleep for 45 minutes. He wakes and seems groggy but ok. My brother expresses concern but my Dad says he is fine, just feeling tired and maybe coming down with something. Goes off to continue his day.
Later that evening my stepmom remains worried about my dad so calls my brother. She says he seems out of breath and has trouble holding a knife and fork at dinner.
My brother advises calling an ambulance right away.
15 minutes later my dad calls my brother and sounds very lucid, saying he is now feeling fine. My brother makes my father promise to visit his GP first thing in the morning. He agrees.
*We now wonder if Dad suffered a TIA that day??*
Monday
Early morning GP appointment, Stepmom accompanies Dad and GP notes breathing difficulty. Takes Temp, which is high. Does an ECG and identifies atrial fibrillation. Listens to chest. Takes bloods. Initial diagnosis of chest infection, Amoxicillin tablets prescribed and asks Dad to keep in touch and come back for follow up examination.
Wednesday
My sister speaks to Dad on the telephone. He says he is feeling better and that the antibiotics are working. He says he is working at home, answering urgent emails. My sister feels that is unusual behavior: normally Dad is very good at self-care and takes himself off to bed to rest.
Different GP rings to ask how Dad is; my stepmom says he is feeling better. “He shouldn’t be. I’m looking at his blood results now. I’m coming out to see him”. GP arrives, isn’t happy with Dad, and sends him to Hospital suspecting Sepsis.
He is admitted to the Acute Unit via Accident & Emergency and put on IV antibiotics, fluids and given oxygen (via mask I think? Or nasal cannula?)
Transferred to Respiratory Ward.
Thursday
Dad tells stepmom and my sister that he was struggling to breathe overnight even with the nasal oxygen tube. Says he was terribly frightened and thought he was going to die. Says he asked the Ward sister to fetch the doctor (my Dad would NEVER ask unless desperate!) but that she would not. My stepmom vows to stay all day and overnight with him.
His breathing deteriorates during the day and by late afternoon a consultant and his team comes down from ICU to assess Dad. Consultant transfers Dad to ICU right away on examination. He explains to my stepmom and brother that they will need to ventilate Dad, but that they will settle him in ICU and that they speak to him for a few minutes before they sedate him.
Consultant comes to the waiting room to tell them that Dad’s breathing deteriorated so much on the way up to ICU that he had to ventilate Dad immediately. Said he was delirious. His blood pressure had plummeted too.
The next few days are critical. The doctors tell my stepmom and family that the infection is so bad they don’t know if Dad will survive. Blood work doesn’t identify the bacteria (it never will, in fact) so they use a combo of two broad spectrum antibiotics.
Different consultant adds a third antibiotic when she learns Dad owns a residential care home for the elderly.
Dad remains on mechanical ventilator for next 7 days. They do sedation holds most days. However, when they lift it too much his heart rate and blood pressure soar. He becomes very distressed, so they turn sedation up again.
His CRP infection markers don’t really come down by much. The consultant team remain concerned.
RECOMMENDED:
Thursday
I fly home early from my holiday in Ohio, leaving my two small children with my husband and his family.
I find Dad very ill, but ‘stable’.
2nd Sunday
They decide to do a CT scan of his lungs. The consultant tells us they are very concerned about the inflammation and scarring to his lungs; that effectively there is no improvement. She says he is effectively in lung failure. She says she is worried about his renal function. She is not optimistic that Dad can survive. Says they will try steroid therapy.
She asks us to consider what kind of life Dad can hope to have if he survived the infection. She said it would mean life in Hospital, on oxygen support, probably in a wheelchair. She says he will be at constant risk of further infections.
There had been a discussion of a tracheostomy, we ask her about it. She says he is too perilously ill to undergo the procedure.
2nd Monday
This week they start Dad on kidney dialysis.
They tell us his bowel movements continue to be diarrhea-like, which concerns them.
He remains on the mechanical ventilator and sedation. He appears to develop a secondary lung infection. They treat with a new antibiotic.
We ask to meet with the consultant microbiologist, who visits the unit daily. He is generous with his time, open and dynamic. He tells us they’ve never been able to identify the source bacteria of Dad’s infection, but that isn’t uncommon. What concerns them more is the inflammatory response Dad is showing. Dad isn’t really responding to the treatment in the usual way. He’s a bit of a puzzle to them.
He asks us to tell him about Dad’s childhood illnesses, travel history, and movements in the days leading up to his illness, just in case it flags up something of relevance. We say we think his sister had TB as a child, and that he was isolated in Hospital aged 2 in case it was incubating it.
He says he wants to do everything he can to help Dad. He even willingly speaks to a friend of the family (a specialist doctor in infectious disease) to kick about ideas. We are very grateful for his openness.
My sister asks the ICU consultant why they aren’t doing scans of his brain and body. She says she is confident it’s a single organ issue.
They tell us his lung failure remains a massive concern.
2nd Monday
Dad’s infection markers have come down. They talk about doing a tracheostomy, which they do on the morning of Friday May 7. Procedure is uneventful and successful. Sedation is withdrawn.
Unfortunately, in the afternoon he suffers 4 cardiac arrests, which they reverse straight away. They take him to ICU lab and fit a temp pacemaker. Cardiologist comes and prescribes medicine. They tell us in asking Dad to do more of the breathing, and less from the machine, his heart couldn’t cope. They tell us it’s multi organ failure and that Dad simply isn’t getting better.
2nd Thursday
Dad suffers another 3 cardiac arrests, which they reverse straight away. We ask about brain damage but are assured the quality of the CPR is good and that his oxygen levels never dropped. They fit a more permanent pacemaker on the front of his chest. His heart stabilizes, and in recent days they are now talking about removing it as they don’t think he needs it apparently.
2nd Friday
We have many conversations with the consultant. They say dad is not waking up, and that he should be. They say they get no response from him when they do the coma tests. In fact, they worry Dad is doing the posturing movement on his arms when they dig at his nails. They tell us they think we should consider withdrawing treatment, and soon. We ask will they consider one last treatment of steroids – they agree.
The whole family gathers round his bed. Then Dad opens his eyes for the first time. We are uncomfortable at the idea of withdrawing treatment. What if Dad is still there? What if he can’t communicate yet? What if he has lost all muscle tone and can’t squeeze hands or move is eyes/head?
Recommended:
We ask to speak to the consultant, who listens to us. My sister and I ask to review Dad’s case right from the beginning. We want to talk to him about the days leading up to Dad’s admission to Hospital, particularly the possibility of a TIA or some kind of neurological event. It becomes clear that, despite our Stepmother outlining dad’s symptoms when he was admitted, a possible TIA/neurological event has been “lost”. The consultant confirms he was not aware of this; only the respiratory issue and sepsis.
We ask could they give Dad more time. He agrees.
On Sunday, the consultant offers an MRI scan of his brain, which floors us. He explains it’s helpful for looking at the intricacies of the brain and the brain stem – they wonder if there is damage there. He also says Dad’s cough reflex has gone, which is a worrying development. (By the next day it’s back, and strong.)
We wonder if it’s the information we have given re a possible neurological event that has prompted a scan? We say yes please.
3rd Monday
Consultant informs us Dad’s pacemaker is not compatible with the MRI – a source of frustration for us. They say they will send him for brain CT scan instead. It comes back showing nothing. We ask would they consider doing a lumber puncture, an EEG, or getting an assessment by a consultant neurologist. They say it’s not something they would normally do in ICU.
They say they will give him time over the next few days and see what that brings.
RECOMMENDED:
3rd Monday to present:
They actually got Dad to breathe on his own, increasing it from one hour each day to 12 hours over a week. The consultant said his saturation levels were actually higher off the ventilator. They admit they are stunned; they thought he could never breathe on his own again.
They decided to speak to a neurologist, who advised a lumbar puncture!! Results came back normal.
His kidneys recovered and he’s off dialysis.
They even took him outside in his chair bed to enjoy the sunshine for 10 minutes.
Dad then started to open his eyes more, turn his head, lift his arms. The physio team confirmed he has lost all muscle strength and come in twice a day: they also get him to sit in a special chair for a few hours each day. Gradually he begins to respond to his name being called- he turns his head. The medical and nursing staff ask him questions and he nods or shakes his head.
He will smile when a joke is made, or hears a familiar voice.
The same consultant who said Dad will not wake up is now saying he thinks Dad might wake up! It’s a lot for us to navigate.
In the last few days he has begun to squeeze our hands, wriggle his toes, bend his knees and shift his shoulders.
However, he is still very spaced out though and struggles to focus his eyes. I feel like he suddenly “sees” me and smiles, but then drifts away.
He seems exhausted a lot of the time, but having said that, looks better.
He was off the antibiotics until a week ago when he developed a Temp and a new secondary lung infection. He was put back on the ventilator to give him a rest, although they have sought to reduce it to the lowest setting again. His CRP markers are now under 100 I think.
As of today, he is sitting up, smiles when people talk to him or shakes/nod head to question. He can grasp our hand too.
Apparently last week they put a valve on his tracheostomy pipe and we’re sure they got a croaky yes and no to questions.
I do hope this isn’t too long winded an account – sincere apologies if so!!!
I would very much like to engage your services and would be very keen to hear your thoughts on my Dad’s case.
I guess also we would like to understand what is happening to Dad in terms of emerging from an induced coma.
Does Dad have critical care neuropathy?
Is a slow progression out of an induced coma normal?
Should Dad be making more progress by now?
Does it take some individuals – especially patients in their 70s – longer to emerge?
Does it indicate brain damage?
Why can’t Dad seem to focus his eyes? Do we need to ask for a further assessment from a neurologist/ophthalmologist?
Has he had a stroke?
RECOMMENDED:
In all, Dad’s care has been outstanding and we have sought to work with the clinicians in a respectful way. We are grateful for their expertise.
However, we are also Dad’s advocates and we have fought for him too when we feel we need to. We are realistic about the long term outlook but we want to understand how we can support Dad if a (partial) recovery is possible.
Many thanks in advance!
RECOMMENDED:
Kind regards,
Anna
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to you and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog“ section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!