Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Loved ones in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED“ and in last week’s episode I answered another question from our readers and the question was
You can check out last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer questions that we get quite frequently as part of my 1:1 consulting and advocacy service!
How Do They Manage My Loved One Who is a COVID Patient in ICU?

SARS-CoV-2, the causative agent of coronavirus disease 2019 (COVID-19), is responsible for the largest pandemic facing humanity since the Spanish flu pandemic in the early twentieth century. Since there is no specific recommended treatment, optimized support is the most relevant factor in the patient’s prognosis.
In the hospital setting, the identification of high-risk patients for clinical deterioration is essential to ensure access to ICU for intensive treatment of severe conditions in a timely manner. Early recognition of the patients who will require ICU admission and will benefit most from it, is of utmost importance.
What are the ICU admission criteria for adult patients infected with COVID-19?
Authorities from the Chinese Center for Disease Control and Prevention reported that, among more than 44,000 confirmed cases of COVID-19, about 81% were asymptomatic or presented mild symptoms such as cough, fever, fatigue, and muscle pain. Although for these cases, home management and self-isolation are the appropriate measures, 14% developed a severe form of the disease and 5% were critical, requiring hospitalization and ICU admission, respectively. [3]
Admission criteria include:
- oxygen requirements equal or superior to 6–8 l/min to reach a peripheral oxygen saturation???90–92%
- respiratory failure
- acute organ dysfunction
- patients at high risk for clinical deterioration:
- Age ? 65 years has been found to be an independent predictor of developing Acute Respiratory Distress Syndrome (ARDS), ICU admission, and mortality in several studies.
- Patients with comorbidities like hypertension, diabetes, chronic obstructive pulmonary disease COPD, chronic kidney disease (CKD), and malignant tumors have been found to have significantly high mortality in patients with COVID-19.
- Moreover, patients with two or more comorbidities have significantly escalated risks of ICU admission, invasive ventilation, and mortality as compared with those who had single comorbidity, and even more so as compared with those without any comorbidity [6]
However, in many countries, due to the shortage of ICU beds, usually only patients requiring intubation and invasive mechanical ventilation were admitted to ICU.
Patients with the severe form of the disease must be closely monitored, since rapidly progression from moderate to severe ARDS may occur. Acute hypoxemic respiratory failure is the most common complication occurring in 60–70% of patients admitted to the ICU.
How is my loved one with Covid-19 treated in ICU?
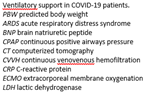
1. Non-invasive ventilation
Many hospitals have adopted non-invasive ventilation (NIV) as an attempt to prevent respiratory failure from evolving into severe forms that require invasive ventilatory support. During this long COVID-19 pandemic outbreak, continuous positive airway pressure (CPAP) and noninvasive ventilation (NIV) are being widely used to treat patients with moderate to severe acute respiratory failure (ARF).
Initially, the treatment for severe respiratory failure included early intubation and invasive ventilation, as this was deemed preferable to be more effective than Non-Invasive Ventilation (NIV). However, emerging evidence has shown that NIV may have a more significant and positive role than initially thought. NIV includes Continuous Positive Airway Pressure or CPAP and Bi-Level Positive Airway Pressure (BiPAP).
Current thinking suggests that NIV and HFNO may be an appropriate bridging adjunct in the early part of the disease progress and may prevent the need for intubation or invasive ventilation. [7]
Positive responses are usually evident soon after the initiation of NIV and HFNC. However, if there is no substantial improvement in gas exchange and respiratory rate within a few hours, invasive mechanical ventilation should be started without delay.
2. Prone position
SARS-CoV-2 virus causes a pneumonia that was identified through fever, dyspnea, and acute respiratory symptoms and named COVID-19. This disease exacerbates in a number of patients and causes pulmonary edema, multi-organ failure, and acute respiratory distress syndrome (ARDS).
Prevalence of ARDS among COVID-19 patients has been reported to be up to 17%. Among the introduced treatment methods for management of ARDS patients, prone position can be used as an adjuvant therapy for improving ventilation in these patients.
Research has found that when proning is used in patients with severe ARDS and hypoxemia not improved by other means, it has the benefit of:
- better ventilation of the dorsal lung regions threatened by alveolar collapse;
- improvement in ventilation/perfusion matching; and
- potentially an improvement in mortality.
Patients remaining in lengthy prone position sessions leads to decrease in mortality of patients. However, correct selection of patients and applying the proper treatment protocol for prone positioning are key to its effectiveness.
3. Intubation for Invasive Mechanical Ventilation
Most of the COVID patients admitted to ICU, will finally require invasive mechanical ventilation (MV) due to diffuse lung injury and acute respiratory distress syndrome (ARDS).
The main objective of mechanical ventilation in these patients is to maintain a lung-protective strategy for all patients with ARDS, defined as targeting a tidal volume of 4 to 8 mL/kg predicted body weight (PBW) and a plateau pressure of less than 30 cmH2O.
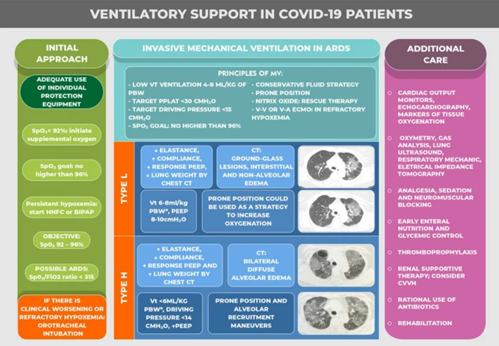
4. Analgesia, Sedation and neuromuscular blockade management in patients with COVID-19
Patients with COVID-19 who undergo mechanical ventilation have an average recovery time of 1–3 weeks. The progress toward improvement is characteristically slow; therefore, prolonged sedation is often unavoidable. In most severe cases of ARDS and also in cases of non-protective ventilation or in the occurrence of asynchrony, neuromuscular blockage is useful, and complications such as polyneuropathy of the critically ill patient are usually diagnosed.
Specifically, neuromuscular blocking agents (NMBA) can be helpful during endotracheal intubation to minimize the risk of patient coughing and possibly infecting healthcare personnel. NMBAs can also be used in patients to promote patient-ventilator synchrony while reducing the driving pressure needed with mechanical ventilation, particularly in patients with the severe clinical presentation.
Prone positioning has also become a cornerstone in managing refractory hypoxemia in patients with SARS-CoV-2 acute respiratory distress syndrome (ARDS), and NMBA can be useful in facilitating this maneuver.
5. Use of Inotropes/Vasopressors
Norepinephrine is the first-line vasopressor in patients with hemodynamic instability and COVID-19. In patients with ARDS, norepinephrine also can improve heart’s RV (Right Ventricular) function by restoring mean arterial pressure and thus RV blood supply.
If norepinephrine is unable to achieve adequate mean arterial pressure, vasopressin could be added as a second-line vasoactive agent to reach the target blood pressure. Vasopressin might be used as first vasopressor, mainly in cases of atrial fibrillation, pulmonary hypertension, and acute renal failure.
6. Antiviral therapy
Several drugs have been studied for the treatment of the SARS-CoV-2. Most studied antivirals in this scenario were the combination of lopinavir–ritonavir and remdesivir. Currently, the antiviral therapy that appears most promising is remdesivir.
Remdesivir has been used recently on a compassionate basis, due to a lack of proven efficacy drugs. A multicenter Randomized Clinical Trial (RCT) including 1063 patients receiving remdesivir or placebo showed that remdesivir use led to a significantly shorter duration of hospital stay (11 vs. 15 days), and lower mortality (8% vs. 11.6%) [11]. The FDA has approved this drug for urgent use in COVID-19.
7. Use of corticosteroids
The use of corticosteroids reduces mortality in COVID-19 patients needing respiratory support. The trial showed that dexamethasone 6 mg once a day for 10 days results in lower 28-day mortality among those who were receiving either invasive mechanical ventilation or oxygen [12].
Patients with severe COVID-19 can develop a systemic inflammatory response that can lead to lung injury and multisystem organ dysfunction. It has been proposed that the potent anti-inflammatory effects of corticosteroids might prevent or mitigate these deleterious effects.
8. Nitric oxide inhalation as an interventional rescue therapy
While there is no specific recommended treatment for COVID-19, nitric oxide has the potential to be of therapeutic value for managing acute respiratory distress syndrome in patients with COVID-19. However, inhaled nitric oxide has not yet been formally evaluated.
Given the extent of the COVID-19 pandemic, and the large numbers of hospitalized patients requiring respiratory support, clinical use of inhaled nitric oxide may become an alternate rescue therapy before extracorporeal membrane oxygenation for the management of acute respiratory distress syndrome in patients with COVID-19.
9. ECMO therapy
Extracorporeal membrane oxygenation (ECMO) is effectively an artificial lung or heart. The technology is used when all other forms of heart and lung support have failed for critically ill patients. It works by temporarily drawing blood from the body to allow artificial oxygenation of the red blood cells and removal of carbon dioxide with a machine.
Now, the treatment is being used to support critically ill patients with Covid-19 pneumonia for whom ventilation is insufficient to sustain blood oxygen levels.
COVID-19 is one of the most challenging health emergencies we have faced this century. Health professionals are experiencing very difficult times, with limitations of resources and information, which when available needs to be confirmed before integration into clinical practice.
To date, there is no proven specific treatment for the management of COVID-19, although studies with promising results have recently emerged. We know already that the lowest rates of mortality are related to better quality of care. Early diagnosis, application of effective therapies and adequate strategies of clinical stratification are needed for better outcomes in COVID-19 patients.
REFERENCES:
1. COVID-19: Critical care and airway management issues
https://www.uptodate.com/contents/covid-19-critical-care-and-airway-management-issues
2. Management of critically ill patients with COVID-19 in ICU: statement from front-line intensive care experts in Wuhan, China
https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-020-00689-1
3. Intensive care management of patients with COVID-19: a practical approach
https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-021-00820-w
4. Treatments for patients with COVID-19
https://www.leedsth.nhs.uk/a-z-of-services/adult-critical-care/covid-19/treatments/
5. COVID-19 Treatment Guidelines
https://www.covid19treatmentguidelines.nih.gov/management/critical-care/oxygenation-and-ventilation/
6. COVID-19 pandemic and the need for objective criteria for ICU admissions
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7262536/
7. COVID-19 disease: Non-Invasive Ventilation and high frequency nasal oxygenation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7261654/
8. COVID-19 Pulmonary Management
https://emedicine.medscape.com/article/2500117-overview#a5
9. COVID-19 Treatment Guidelines: Corticosteroids
https://www.covid19treatmentguidelines.nih.gov/therapies/immunomodulators/corticosteroids/
10. Extracorporeal organs could save the sickest patients from Covid-19
https://www.medicaldevice-network.com/features/ecmo-covid-19-2/
11. Remdesivir for the Treatment of Covid-19 — Final Report
https://www.nejm.org/doi/10.1056/NEJMoa2007764
12. Effect of Dexamethasone on Days Alive and Ventilator-Free in Patients With Moderate or Severe Acute Respiratory Distress Syndrome and COVID-19The CoDEX Randomized Clinical Trial
https://jamanetwork.com/journals/jama/fullarticle/2770277
13. Image credit to:
14. VENTILATORY SUPPORT IN COVID-19 PATIENTS image credit to:
https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-021-00820-w/figures/2
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to Eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to you and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!