What is a shock?
Circulatory shock, commonly known simply as shock, is a life-threatening medical condition with severe effects on the cardiovascular system. In the early stages this is generally manifested in an inadequate tissue level supply of blood flow, oxygen and nutrients to the body’s main and vital organs such as the brain, heart, lungs, kidneys and liver. When checking a person’s blood pressure who is in shock, the reading tends to be very or extremely low, which is also known as hypotension.
The typical signs of shock are low blood pressure, a rapid heartbeat and signs of poor end-organ perfusion or “decompensation/peripheral shut down”, such as low urine output, confusion or loss of consciousness. There are times that a person’s blood pressure may remain stable, but may still be in circulatory shock, so it is not always a sign.
Circulatory shock should not be confused with the emotional state of shock, as the two are not related. Circulatory shock is a life-threatening medical emergency and one of the most common causes of death for critically ill people. Shock can have a variety of effects, all with similar outcomes, but all relate to a problem with the body’s circulatory system. For example, shock may lead to hypoxemia (a lack of oxygen in arterial blood) or cardiac arrest.
One of the key dangers of shock is that it progresses by a positive feedback mechanism, which can lead to a vicious cycle. Once shock begins, it tends to make itself worse. This is why immediate treatment of shock is critical.
- What does the cardiovascular system do?
- Poor or abnormal function
- Causes
- What happens in Intensive Care
- How long will my loved one stay in Intensive Care?
What does the cardiovascular system do?
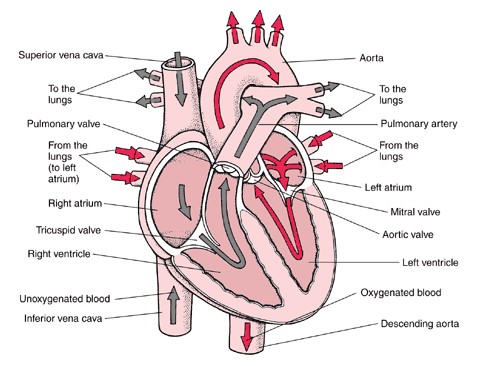
The essential components of the human cardiovascular system are the heart, lungs, blood, and blood vessels. It includes: the pulmonary circulation, a “loop” through the lungs where blood is oxygenated and the systemic circulation, a “loop” through the rest of the body to provide oxygenated blood. An average adult contains five to six quarts (roughly 4.7 to 5.7 liters) of blood, accounting for approximately 7% of their total body weight. Blood consists of plasma, red blood cells, white blood cells, and platelets. Also, the digestive system works with the circulatory system to provide the nutrients the system needs to keep the heart pumping.
The heart is at the centre, basically distributing blood from the ‘central pump’ with the blood vessels the pipes of the body, trying to reach every corner of the body. The cardiovascular system also passes nutrients (such as amino acids, electrolytes and lymph), gases(Oxygen and Carbon Dioxide), hormones, blood cells, etc. to and from cells in the body to help fight diseases, stabilize body temperature and pH, and to maintain blood pressure.
In the heart there is one atrium and one ventricle for each circulation, and with both a systemic and a pulmonary circulation there are four chambers in total: left atrium, left ventricle, right atrium and right ventricle. The right atrium is the upper chamber of the right side of the heart. The blood that is returned to the right atrium is de-oxygenated (poor in oxygen) and passed into the right ventricle to be pumped through the pulmonary artery to the lungs for re-oxygenation(inhalation) and removal of carbon dioxide(exhalation). The left atrium receives newly oxygenated blood from the lungs as well as the pulmonary vein which is passed into the strong left ventricle to be pumped through the aorta to the different organs of the body.The left side of the heart then receives oxygen rich blood from the lungs and pumps this blood into the Aorta and arteries of the body. This pumping action is a complex well-coordinated activity that cannot be fully explained here. The heart itself, receives oxygenated blood supply via the left and right coronary arteries.
Poor or abnormal function of the cardiovascular system
May be a result of:
- Insufficient blood supply due to dehydration, bleeding or swelling;
- Insufficient blood supply to the heart due to ‘clotted’ arteries
- A poor blood supply to the heart, where there is not enough oxygen and other nutrients for its work;
- Poor lung function or obstruction to blood flow in the lungs, which places a strain on the heart muscle;
- Too many or too few electrolytes (eg. potassium, magnesium) that cause irregular heartbeats or dangerous rhythms in the heart.
- Weakness of blood vessel walls
- Heart muscle weakness Cardiomyopathy
- unhealthy lifestyle such as alcohol consumption, smoking, obesity
Shock has different causes.
- Hypovolemic Shock is a state of decreased blood volume, usually caused by a loss of large amounts of blood or body fluids. It is usually caused by serious accidents, during major surgery, in burns and with medical conditions where there is severe vomiting and diarrhoea. In order to compensate for the reduced blood volume a person’s heart will pump faster to try and compensate for the decreased blood volume, resulting in a high heart rate or pulse.(tachycardia)
- Cardiogenic shock occurs as a result of inadequate circulation of blood due to primary failure of the ventricles of the heart to function effectively, usually caused by heart muscle damage. Heart muscle damage usually is a result of a heart attack or when the heart muscle has a severe infection. The damaged heart muscle often results in abnormal heart rates and irregular rhythms(AF, SVT, VF,VT). The heart may also beat too fast (tachycardia) or too slow (bradycardia). Drugs (inotropes) may be needed to help the heart muscle to pump with more force. Cardiogenic shock is a largely irreversible condition and as such is more often fatal than not.The condition involves increasingly more pervasive cell death from lack of oxygen(hypoxia) and nutrient starvation (e.g. hypoglycemia). Because of this it may lead to Cardiac Arrest (or circulatory arrest) which is an acute cessation of cardiac pump function. Cardiogenic shock is defined by sustained hypotension with tissue hypoperfusion despite adequate left ventricular filling pressure. Signs of tissue hypoperfusion include minimal Urine Output (<30 mL/h), cool extremities, and altered level of consciousness.
- Septic shock is caused by severe infection and sepsis. It can cause multiple organ failure and death. Sepsis is the body’s reaction to the toxins (poison) released by the bacteria into the blood. In severe septic shock blood vessels may dilate or constrict. Volume administration, Antibiotic Therapy and Drugs (vasoconstrictors) can be used to narrow the blood vessels whilst other drugs (vasodilators) can be used to open the blood vessels.
- Anaphylactic Shock is a serious allergic reaction caused by a severe allergic reaction that can cause death. It typically causes a number of symptoms including an itchy rash, throat swelling, and low blood pressure. Common causes include insect bites/stings, foods, and medications. In a severe allergic reaction the small blood vessels known as capillaries ‘leak’ fluid and the blood vessels dilate. Usual treatment for this type of shock includes adrenaline.
- Spinal shock is caused by damage(disruption) to the nervous system (brain or spinal cord). The (autonomic) nervous system keeps the muscles of blood vessels slightly contracted, when a part of this system is damaged, those blood vessels lose the ability to constrict and instead they dilate causing shock. Hypotension(low blood pressure) occurs due to decreased systemic vascular resistance resulting in pooling of blood within the extremities lacking sympathetic tone. Bradycardia results from unopposed vagal activity and has been found to be exacerbated by hypoxia(lack of oxygen) and endobronchial suction.
Severe shock usually requires admission to an Intensive Care Unit.
What happens in Intensive Care?
Treatment for your loved one who has suffered a severe shock may be straightforward or quite complex depending on the individual Patient and their immediate condition after the shock. Investigations such as blood tests(Blood& Pathology tests in Intensive Care), Chest X-ray, CT, ultrasound of the heart(Echoecardiography)etc… are performed to identify the cause of the shock and treatment will be commenced accordingly. Further investigations will be required if your loved one does not regain consciousness in a short time.
- Initially oxygen and respiratory support might be commenced via na oxygen mask or via Non- Invasive Ventilation(NIV) or BIPAP ventilation
- Full ventilation using a Ventilators(Breathing Machine) and a Breathing Tube (endotracheal tube) will usually be required to improve and maintain the oxygen delivery
- Sedation may be used if your loved one is in an induced coma
- Your loved one will require monitoring using a Bedside Monitors and an Arterial Catheter(Arterial Line)
- You can expect your loved one to have frequent Chest X-rays and blood tests(Blood& Pathology tests in Intensive Care) especially arterial blood gases (ABGs)
- Infusion pumps are administering drugs to support your loved ones blood pressure and haemodynamic system, as well as intravenous fluids may be administered via a central venous catheter/ CVC(Central Venous Lines)
- Use of a Pulmonary Artery Catheters or a PICCO catheter to closely monitor cardiac function is not uncommon.
- An NG Tube (Nasogastric Tubes) is usually inserted into your loved ones stomach, in order to commence nutrition or to remove fluids
- Urine Output is usually measured hourly, after insertion of a Urinary Catheter
- Fluid therapy is essential and can be given including:
- Crystalloids – salt, water and electrolyte solutions
- Colloids – ‘plasma’ like solutions
- Blood and blood products(Red blood cells, FFP’s= Fresh Frozen Plasma, Platelets etc…)
- Drugs – to restore abnormal body functions.
- Inotropes(Dobutamine/Dobutrex, Milrinone) – to assist the heart to pump with more force at the right rate
- Vasodilators(GTN, Sodium Nitroprusside(SNP)) – to open up blood vessels
- Vasoconstrictors(Noradrenaline, Adrenaline) – to narrow blood vessels
- Antibiotics – to fight infection caused by bacteria
Surgery – to control bleeding (hemorrhage) due to severe injuries
The information contained in this sheet is general in nature and therefore cannot reflect individual patient variation. It is provided as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one.
How long will your loved one remain in ICU?
Your loved one will remain in intensive care while they have investigations and treatment. Each Patient’s condition is very unique and especially with varying types of shock, the length of stay can vary from a few days up to weeks or sometimes even longer. It is important to speak with the medical and nursing team caring for your loved one to discuss the potential outcome and prognosis.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
Related Articles:
- How long should a Patient be on a ventilator before having a Tracheostomy?
- How long can a breathing tube or an endotracheal tube can stay in?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Why does my loved one need a Tracheostomy in Intensive Care?
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- Be more selfish if your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 4 ways on how to be more persuasive if your loved one is critically ill in Intensive Care
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- How long does it take to wake up from a Traumatic brain injury or severe head injury
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure



