What is Adult Respiratory Distress Syndrome (ARDS)?
Acute respiratory distress syndrome (ARDS), also known as respiratory distress syndrome (RDS) or Acute Lung Injury (ALI) is a serious reaction to various forms of injuries or acute infection to the lung. ARDS is a severe lung syndrome (not a disease) caused by a variety of direct and indirect issues. It is characterized by inflammation of the lung parenchyma (tissue) leading to impaired gas exchange with concomitant systemic release of inflammatory mediators causing inflammation, hypoxemia and frequently resulting in multiple organ failure. This condition is often fatal, usually requiring mechanical ventilation and admission to an intensive care unit.
ARDS is often caused by lung contusions, severe pneumonia, aspiration of gastric/ stomach content, severe infections, massive blood transfusions, pancreatitis, severe trauma or burns.
Those disturbances can cause the body to leak fluids from the veins or arteries into the lungs, causing Pulmonary Oedema, by having excess fluids in the lungs, making a gas exchange (oxygenation) almost impossible. This process can take a few hours or can occur over a number of days.
- What does the Respiratory system do?
- Abnormal and or inadequate breathing
- What Happens in Intensive Care?
- How long will my loved one remain in Intensive Care?
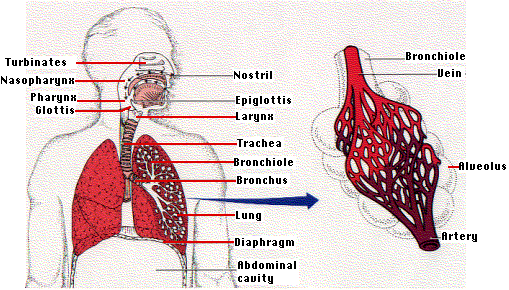
What does the Respiratory System do?
The respiratory system consists of the lungs, airways and blood vessels. The respiratory system inhales oxygen into the body and exchanges oxygen by removing carbon dioxide from the body. A normal breath requires a complex coordination between the nervous system (brain & spinal cord) and the muscles of breathing (including the diaphragm and muscles between the ribs).
Abnormal and or inadequate breathing can occur as a result of:
- An interruption to the nervous system (head injuries or spinal injuries for example)
- Barriers to the absorption of oxygen (eg fluid or secretions in the alveoli);
- Obstruction to the flow of gases through the lungs, both breathing in or out (eg asthma);
- Damage to the rib cage such as rib fractures or flail chest (in motor vehicle trauma for example);
- Pneumothorax (deflation of one part of the lung)
- Haemothorax (infiltration with blood to parts of the lung)
- Pain, which makes taking a normal breath difficult
A number of respiratory conditions can result in respiratory failure and require Intensive Care or High dependency Unit admission. It is often that respiratory failure results in ventilation support (help with breathing). This support may be through the use of oxygen masks, BIPAP or Non- Invasive Ventilation (NIV) or via a Breathing Tube (endotracheal tube) and Ventilators (Breathing Machines)
What happens in Intensive Care?
Your loved one can be admitted to an intensive care because it is thought they have or may be developing ARDS, but it is more likely that they are Patient in Intensive Care already for other reasons. The treatment for ARDS revolves around supporting the lungs until they can repair themselves.
In acute respiratory distress syndrome (ARDS), overproduction of inflammatory factors in lung tissue is followed by pulmonary edema and severe hypoxemia and an increase in pulmonary dead space. Despite significant advances in our understanding and management of patients with ARDS, the morbidity and mortality associated with ARDS remains high. Few measures have been proven to improve outcomes in ARDS.
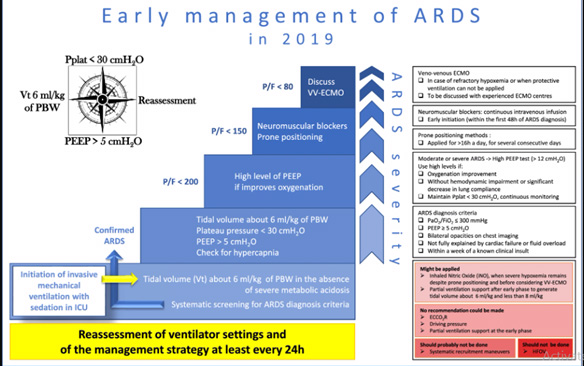
Recommendations for the management of adult patients with acute respiratory distress syndrome (ARDS):
 OXYGEN AND VENTILATION
OXYGEN AND VENTILATION
The decision to initiate some treatments is taken after a “stabilization” phase that includes optimization of mechanical ventilation as the first step of management. Oxygen saturation should be maintained between 88% and 95%, which usually requires mechanical ventilation with titration of inspired oxygen (FiO?). Occasionally patients can be managed with non-invasive ventilation, but the failure rate is high and the majority will require endotracheal intubation. Data regarding the use of high-flow oxygen via nasal cannula (HFNC) in patients with acute hypoxaemic respiratory failure are inconsistent; the safety and efficacy of HFNC in patients with ARDS has not been studied prospectively.
Ventilator-associated lung injury may be limited by the use of a low tidal volume (amount of air breathed in with each normal breath), plateau-pressure-limited protective ventilatory strategy. This therapy has been shown to reduce mortality. Recently, it has been demonstrated that mechanical ventilation by lung protection strategy can be provided in patients with ARDS, resulting in better pulmonary function and higher rates of weaning from the ventilator. The nearly maximal alveolar recruitment and aeration accomplished with this strategy were intended to minimize shear stresses in the lung tissue during inspiration.
- PRONE POSITIONING RECOMMENDED 12 HRS PER DAY FOR MODERATE / SEVERE ARDS
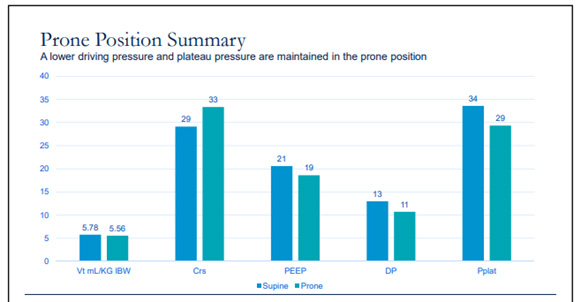
Prone positioning can improve oxygenation in patients with ARDS and has been shown to reduce mortality in patients with severe ARDS. One systematic review found that reduced mortality was contingent upon patients remaining prone for at least 12 hours daily.
A case example in ARDS and respiratory failure during Live Ventilator Management Workshop in the US is shown below integrating recreated live simulated clinical scenario via a high-fidelity lung model to a live audience that illustrates the effect of prone positioning on respiratory system using a live simulator. (1)
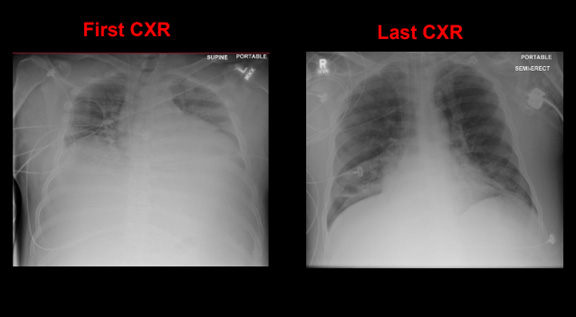
SUMMARY OF HOSPITAL COURSE: 66 days of MV § 48 days of prone positioning § 53 days to spontaneous breathing § 12 days of spontaneous breathing pre extubation
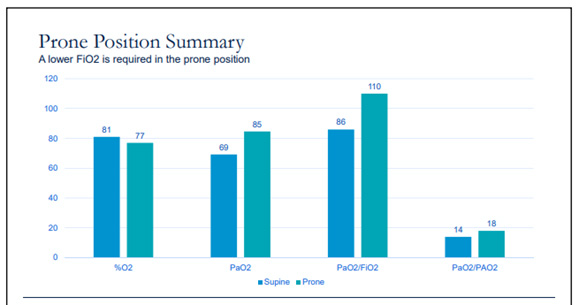
Given the potential complications of prone positioning, including facial edema, pressure sores, and dislodgement of catheters and endotracheal tubes, prone positioning should only be considered in patients with severe ARDS.
 INTRAVENOUS FLUIDS
INTRAVENOUS FLUIDS
The patient’s fluid balance should be maintained as slightly negative or neutral (providing the patient is not in shock). A central line is recommended to measure the central venous pressure (CVP), with regular assessments of fluid status. The goal is to keep the CVP <4 cm H?O. The routine use of a pulmonary artery catheter (to measure pulmonary artery occlusion pressure) is not recommended as insertion is associated with more complications than a central line. The use of a conservative fluid management strategy was suggested for all patients.

- ANTIMICROBIALS + IDENTIFICATION AND TREATMENT OF SOURCE OF INFECTION
In patients who have an infectious cause for ARDS (e.g., pneumonia or sepsis), the prompt initiation of antimicrobials is important. Empirical antibiotics targeted at the suspected underlying infection should be used as soon as possible after obtaining appropriate cultures including blood, sputum, and urine cultures. Antivirals or antifungals may be appropriate in patients with suspected viral or fungal infections. Once culture results are available, the antimicrobial regimen can be tailored for the identified organism. There is no evidence to support the use of antibiotics in patients who have ARDS without infection.
- NEUROMUSCULAR BLOCKING AGENT CISATRACURIUM FOR 48 HRS FOR SEVERE ARDS
Neuromuscular paralysis improves ventilator-patient synchrony and often improves oxygenation. In a randomised trial in patients with severe ARDS, 48 hours of neuromuscular paralysis with cisatracurium improved oxygen and improved mortality with no increase in intensive care unit-related paresis. Neuromuscular paralysis should be instituted when adequate oxygenation (oxygen saturation >88% to 95%) cannot be achieved despite low tidal volume ventilation and adequate sedation, particularly if there is still evidence of ventilator-patient dyssynchrony. Intermittent doses of paralytics can be used as effectively as a continuous intravenous infusion.
- HIGH FREQUENCY OSCILLATION WAS NOT RECOMMENDED
Routine use of high-frequency oscillatory ventilation (HFOV) in moderate-to-severe ARDS is not beneficial, and may be harmful. However, HFOV may still have a role as a rescue therapy for patients with severe ARDS and refractory hypoxaemia, because the use of HFOV often improves oxygenation.
- SUGGESTED THAT INHALED NITRIC OXIDE IS NOT USED
Inhaled nitric oxide can improve oxygenation in patients with ARDS, but does not improve mortality and has been associated with acute kidney injury thus they should be used mainly as a rescue therapy only after traditional treatments fail, rather than as standard care in ARDS.
A study showed randomized trials of inhaled nitric oxide in 1,069 patients with ARDS showed that inhaled nitric oxide had no effect on mortality in ARDS, even in the most hypoxemic patients. (6). Inhaled prostacyclin is easier to administer than inhaled nitric oxide, and also has the potential to improve oxygenation in ARDS through better ventilation perfusion matching. However, there are currently no published large randomised controlled trials of inhaled prostacyclin; thus, it should be used cautiously and only as a rescue therapy.
The authors of this article have in their intensive care practice experienced nitric oxide and prostacyclin nebuliser as a therapy option in ARDS with varied results.
- EXTRACORPOREAL MEMBRANE OXYGENATION (ECMO) AS AN ADJUNCT
Extracorporeal membrane oxygenation was suggested as an adjunct to protective mechanical ventilation for patients with very severe ARDS. in whom standard therapies are failing (i.e., patients with profound refractory hypoxaemia). In patients with severe acute ARDS, venovenous ECMO is associated with reduced 60-day mortality compared with conventional mechanical ventilation, despite a moderate risk of major bleeding.
SUPPORTIVE CARE
Standard supportive care of critically ill patients includes:
- Prevention of deep vein thrombosis
- Blood glucose control
- Prophylaxis against stress-induced gastrointestinal bleeding
- Haemodynamic support with inotropes / vasopressors to maintain a mean arterial pressure >60 mmHg
- Transfusion of packed red blood cells in patients with haemoglobin <70 g/L (<7 g/dL).
- Nutrition should be provided enterally where In a large randomised trial in 1000 patients with ARDS low-dose enteral feeding for the first 5 days of ARDS had similar clinical outcomes compared with full-calorie feeding.
- Inhaled or intravenous beta-adrenergic agonists to promote alveolar fluid clearance and resolution of pulmonary oedema are not recommended.
- Neither early nor late administration of corticosteroids has been shown to improve mortality in patients with ARDS, and their routine use is not recommended.
- Tracheostomy ventilation whenever prolonged ventilation (>2 weeks) is deemed inevitable
- Your loved one will require monitoring using a Bedside Monitors and an Arterial Catheter (Arterial Line)
- You can expect your loved one to have frequent Chest X-rays and blood tests (Blood& Pathology tests in Intensive Care) especially arterial blood gases (ABGs)
How long will your loved one remain in Intensive Care?
Your loved ones prognosis and length of stay in intensive care is closely linked to the severity of the ARDS, failure of other organs (especially the kidneys, liver, heart and brain) and whether he or she has an infection. The survival rate is around 65%. Patients who survive ARDS, usually fully recover, however it is a long and slow process.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual Patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
REFERENCES:
- Case examples in ARDS and Respiratory Failure, Jan. 18, 2019
https://calthoracic.org/wp-content/uploads/2019/01/07-CTS_ARDS-Case-Final.pdf
- GUIDELINES ON THE MANAGEMENT OF ACUTE RESPIRATORY DISTRESS SYNDROME
https://www.ficm.ac.uk/sites/default/files/ficm_ics_ards_guideline_-_july_2018.pdf
- Guidelines on the management of acute respiratory distress syndrome
https://bmjopenrespres.bmj.com/content/6/1/e000420.full
- Formal guidelines: management of acute respiratory distress syndrome, June 04, 2019
https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-019-0540-9
- Acute respiratory distress syndrome, Last updated: October 2019
https://bestpractice.bmj.com/topics/en-gb/374/treatment-algorithm#patientGroup-0-0
- Epitaph for nitric oxide for ARDS
https://pulmccm.org/ards-review/epitaph-nitric-oxide-ards-crit-care-med/
- Inhalation therapies in acute respiratory distress syndrome
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5537120/
- Lung protection strategy as an effective treatment in acute respiratory distress syndrome


