Common Blood and other Pathology Tests in the Intensive Care Unit
In order to identify actual or impending problems and to monitor the effectiveness of treatments and change in conditions, Patients in Intensive Care require a wide variety and frequent pathology tests on different body fluids (E.g. blood, sputum and urine).
- Why so many different tests and so often?
- How are the tests done?
- Who will explain the results to me?
- EUC -Electrolytes (Sodium/ Potassium/ Chloride)/ Urea/ Creatinine
- Arterial Blood Gas – ABG
- Liver Function Tests – LFTs
- Full Blood Count – FBC
- Coagulation Studies – Coags
- Blood sugar level- BSL
- Urinalysis
- Pathology Tests to identify possible infection
- Blood Cultures
- MSU – mid stream urine test
- Sputum Specimen
- Wound Swabs
- CSF -Cerebrospinal Fluid(Fluid in the brain and spine)
- Other body fluids
Why do Intensive Care Patients and my loved one have lots of blood tests?
Patients in Intensive Care are critically ill and their condition is usually fragile. In order to identify, optimise and alter treatment, critically ill Patients will have a wide variety of Pathology tests on different body fluids (E.g. blood, sputum and urine).
Why so many different tests and so often?
The types of tests and how often these tests are performed depend on why the Patient is in ICU, drugs and medication your loved one receives and how unwell your loved one is. Blood tests are usually done on admission to the ICU and then on a daily basis. However some tests will be repeated 3 or 4 times a day, depending on circumstances.
How are the tests done?
Because of the increased frequency of pathology tests required in Intensive Care, an arterial line(Arterial Catheter) is often used to minimise your loved ones discomfort from repeated blood drawings. Unfortunately, some tests cannot be done using an arterial line. All staff taking blood tests are trained to minimise Patient discomfort when performing these tasks. The most common tests are described below.
Who will explain the results to me and my loved one?
In most cases you can expect a general explanation of the blood results of your loved one from the doctors and the nurses. They will explain whether results are normal or abnormal without going into too much detail, as it is difficult to understand the large number of blood tests and the results without formal education. Results that are detrimental to your loved ones condition and/or recovery will be explained to you. The most common ones would be Haemoglobin(HB or red blood cells) or deteriorating renal/kidney function(urea and creatinine)
If you have further questions please ask the nurses and doctors caring for your loved one.
Blood Tests
EUC – Electrolytes (Sodium/Potassium/Chloride)/Urea/Creatinine
The test is often used as a screening test for Patients who are critically ill in ICU, to detect abnormalities of blood chemistry, including kidney failure and dehydration.
How the Test is Performed
The EUC test is a blood test and requires a few millilitres of blood from an artery or vein. In newborn babies blood may be taken from a heel-prick sample.
Medical Conditions and Symptoms
EUC is usually performed to confirm normal kidney function (renal function) in Urea and Creatinine or to exclude a serious imbalance of biochemical salts in the bloodstream. A diverse number of conditions may be detected on the EUC test, as each parameter tested may be high or low.
This test involves taking between1-4 mls of blood from either a vein or an artery. This test looks at the basic chemical balance of the blood as well as kidney function. An imbalance in the chemical makeup of the blood will occur in a number of circumstances. This test will also indicate whether replacement of a body salt is required. Urea and creatinine are a direct measure of how well the kidneys are working.
Tests in ICU are usually done on a daily basis, ore often, if the Patient requires Haemodialysis with Dialysis Machines
The results are usually available in 1-2 hrs.
This is a picture of a patient having blood taken from a vein in the elbow. It was found using a google image search at this Website.

Arterial Blood Gas – ABG
An arterial blood gas (ABG) is a blood test that is performed using blood from an artery. It involves puncturing an artery with a thin needle and syringe and drawing a small volume of blood. The most common puncture site is the radial artery at the wrist, but sometimes the femoral artery in the groin or other sites are used. In Intensive Care the blood is normally drawn from an Arterial Catheter. An ABG is a test that measures the arterial oxygen tension (PaO2), carbon dioxide tension (PaCO2), and acidity (pH). In addition, arterial oxyhemoglobin saturation (SaO2) can be determined. Such information is vital when caring for Patients with critical illness or respiratory disease. As a result, the ABG is one of the most common tests performed on Patients in intensive care units (ICUs).
The test is used to determine the pH of the blood, the partial pressure of carbon dioxide and oxygen, and the bicarbonate level. Many blood gas analyzers will also report concentrations of lactate, hemoglobin and several electrolytes., ABG testing is mainly used in critical care medicine to determine gas exchange which reflect gas exchange in the lungs.
This test involves taking a small amount of blood, around 1-2 mls from an artery.
Examples of conditions where this is important could include Pneumonia, poorly controlled diabetes, cardiac failure and renal failure(Acute Kidney(Renal) Failure)

This is a picture of a patient having an ABG taken from the radial artery. Picture found using google image search at this Website
- Most Patients in ICU, including your loved one, will require at least one ABG, usually on admission. If your loved one requires Non- Invasive Ventilation(NIV) or BIPAP ventilation or requires a Breathing Tube (endotracheal tube) and mechanical ventilation on Ventilators (Breathing Machines) this test is done more frequently, sometimes every 2-4 hours. The results are usually back within a few minutes.
Liver Function Tests – LFTs
Blood to do this test is included in a sample taken for EUC. Liver function tests (LFTs or LFs), are groups of clinical biochemistry laboratory blood designed to give information about the state of a Patient’s liver. This test gives a picture of the liver function.
Cardiac Enzymes – CE
Cardiac Enzymesare markers measured to evaluate heart function. They are often discussed in the context of Heart Attack(Acute Myocardial Infarction) but other conditions can lead to an elevation in cardiac marker level.
Most of the early markers identified were enzymes, and as a result, the term “cardiac enzymes” is sometimes used. CK and troponin are the two most commonly measured, especially if there is suspicion that the cardiac muscles have been damaged. CE’s are usually done several times in the first 24 hours if a cardiac incident is suspected. For Patients admitted to the coronary care unit (CCU) CE are usually done on a regular basis.
Full Blood Count – FBC
As the name suggests this test ‘counts’ the number of each of the different blood cells in the blood.
Haemoglobin or ‘Hb’ are the red blood cells, carrying oxygen around the body. A reduced Hb is called anaemia. A blood transfusion may be required if the Hb is too low. The white cell count (WCC) is an indication of infection or inflammation in the body. Platelets form an integral part of the clotting mechanism of the blood.
A FBC is usually done on admission and then daily. If blood transfusions are required or there is a concern regarding bleeding the FBC will be done more frequently.
Coagulation Studies – Coags
Coagulation profile(Coag) includes INR, APTT, Platelets and fibrinogen. it’s a screening test for abnormal blood clotting because it examines the factors most often associated with a bleeding problem.
How the Test is Performed
Coagulation profile is a blood test. It requires a few milliliters of blood from a vein, and it is important that the blood sample tube is filled to the correct level – otherwise false readings may occur.
Medical Conditions and Symptoms
A Coagulation profile may be performed to confirm normal clotting function before a procedure which may cause bleeding, or in conditions associated with bleeding, for example from the respiratory, urinary, or gastrointestinal tract. This may happen because of hereditary conditions such as Haemophilia, or acquired conditions such as liver failure, or severe infections. A condition called Disseminated Intravascular Coagulation (DIC) may occur in critically ill Patients, from a variety of possible causes. DIC affects all the components of the coagulation profile. Envenomation from some types of snakebite may also cause a coagulopathy – an abnormality of the normal clotting process. Warfarin therapy is a medical cause of easy bleeding, and shows up in the INR component of the coagulation profile.
This blood test evaluates the blood’s clotting status. Regular coagulation studies are required when a Patient is receiving anti-clotting drugs such as heparin or warfarin. In ICU the test is done on admission and then daily unless the coagulation status is abnormal. When starting a heparin infusion or commencing warfarin therapy frequent testing may be required before the right dosage is established. This may mean a number of tests per day. If in place an arterial line(Arterial Catheter) can be used.
Blood sugar level – BSL
Abnormal blood glucose levels are common during critical illness, as stress levels are high and high stress levels are associated with higher blood sugar levels, even for non- diabetics.
A BSL in Intensive Care can be done in different ways. The blood specimen may be obtained from a specimen used for a EUC or an ABG or using the ‘stab’ on finger method. The test is generally done at the Patient’s bedside using a small glucometer. If BSL are stable the test is done once or twice a day. The BSL will be done more frequently and as required if your loved one is diabetic, the BSL is unstable and your loved one requires an Insulin infusion, as is often the case in Intensive Care. Therefore a tight control of the BSL is required, especially since many factors are at play that impact on the BSL.
Other Tests
Urinalysis
A urinalysis (UA), is a routine test performed on urine, and one of the most common methods of medical diagnosis.
The target parameters that can be measured or quantified in urinalysis include many substances and cells, as well as other properties, such as specific gravity. Since most critically ill patients have a urinary catheter in place obtaining a clean specimen is quite easy.
Only a small amount of Urine is sufficient for accurate testing, which can indicate a number of abnormalities including infection, dehydration, abnormal kidney or liver function, presence of glucose or ketones or blood.
A part of a urinalysis can be performed by using urine test strips, in which the test results can be read as color changes. Another method is light microscopy of urine samples.
Results are usually back within 1-2 days. If there is a suspicion that the renal (kidney) system is the source of a possible infection broad spectrum antibiotics will be started until the infective organism is identified
Pathology Tests to identify possible infection
A septic screening for possible sources of infections are usually done on Patients with a high or increasing temperature(Fever) or Patients who have been in ICU for a lengthy period, as a routine check. A septic screening therefore normally involves blood cultures, a sputum sample, a urine specimen and samples from any other areas such as wounds or access lines(Arterial Catheter and Central Venous Lines)
Blood Cultures
Blood cultureis a microbiological culture of blood. It is used when infections are suspected, to detect infections that are spreading through the bloodstream (such as bacteremia, septicemia amongst others). This is possible because the bloodstream is usually a sterile environment. The purpose of blood cultures are, when a Patient shows signs or symptoms of a systemic infection, results from a blood culture can verify that an infection is present, and they can identify the type (or types) of microorganism(bacteria) that is responsible for the infection. For example, blood tests can identify the causative organisms in severe Pneumonia, puerperal fever, pelvic inflammatory disease, neonatal epiglottitis, sepsis, and fever of unknown origin (FUO). However, negative growths(no growth in bacteria) do not exclude infection. Once the causes of infections have been determined, the right Antibiotic therapy can be chosen and the progress of antibiotic treatment can be monitored. Usually it required two sets of testing initially, followed by further tests as required.
A preliminary result will be available within several hours however the final results from a blood culture can take several days. If a patient is quite sick with a suspected infection antibiotics will be started before the full test results are available. This antibiotic regime may then be adjusted when the full results are available. Unfortunately, it is not always possible to identify the cause of the infection.
 A picture of typical blood culture bottles
A picture of typical blood culture bottles
MSU – mid stream urine test
Please see Urinalysis
Sputum Specimen
Sputum is mucus that is coughed up from the lower airways. In medicine, sputum samples are usually used for microbiological investigations of respiratory infections and cytological investigation of respiratory systems.
The lungs are quite often the source of an infection in the intensive care patient. There is normally a number of organisms in the throat and upper airways of a person. The presence of organisms in the sputum of a Patient or your loved one does not necessarily mean that the Patient or your loved one has pneumonia. A sputum specimen can be obtained in a number of ways. Ideally the sputum specimen may be obtained from deep inside the lungs. If your loved one is ventilated, he or she will be suctioned with a clean suction catheter. If your loved one is not ventilated he or she can cough up some sputum in a container for testing. Sometimes, to obtain the optimal sample a Bronchoscopy may need to be done. Alternatively, a Bronchi Alveolar Lavage may be performed for testing.
Wound Swabs
If a wound, such as an abrasion or surgical incision, appears infected, a wound swab is usually taken. This involves cleaning the wound with normal saline and ‘wiping’ a sterile swab across the wound. The swab is taken to the microbiology laboratory for testing. Results take several days. If the wound is highly likely to be the source of infection or sepsis, usually a Broadband Antibiotic therapy is commenced before the actual results are back.
CSF – Cerebrospinal Fluid
CSF is is a clear colorless bodily fluid produced in the brain. It acts as a cushion or buffer for the cortex, providing a basic mechanical and immunological protection to the brain inside the skull and serves a vital function in cerebral(brain) auto regulation of cerebral(brain) blood flow.
CSF bathes the brain and spinal cord. A specimen of this fluid is obtained when infection such as Meningitis or Encephalitis is suspected. A lumbar puncture may be performed to extract some CSF. This procedure involves inserting a needle between two vertebrae in the lower back under sterile conditions and a small amount of CSF is drained and sent to the laboratory for the identification of infection and other abnormalities. The other option to extract CSF for testing is if your loved one has an intraventricular drain(Intracranial Pressure Monitoring) insitu, CSF can be taken out of the drain and sent for testing.
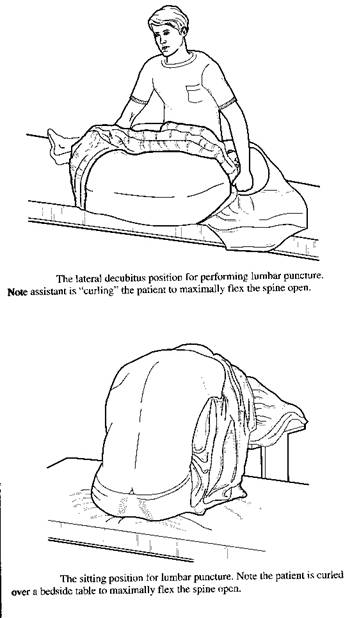 These pictures demonstrate the two common positions a Patient may be in for a lumbar puncture. The ICU patient will generally be lying down. The picture was found using a google image search at the following Website.
These pictures demonstrate the two common positions a Patient may be in for a lumbar puncture. The ICU patient will generally be lying down. The picture was found using a google image search at the following Website.
Other body fluids
Samples of fluids from other parts of the body may be sent for examination if they could be the source of infection. If the Patient or your loved one has a drain in place a sample from this site is easily obtained (E.g. intercostal catheter).
There is a very long list of blood and other tests, which are carried out on Intensive Care Patients. However it is beyond the capacity of this site to list and describe them all. Please ask the medical and nursing staff caring for your loved one to explain any additional tests that have been done.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual Patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
How can you have PEACE OF MIND, control, power and influence whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below! In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care! Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below!
In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care!
In your FREE reports you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 “killer” tips& strategies helping you to get on the right path to PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘BEHIND THE SCENES’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care(it’s not what you think)
Make sure you also check out our “blog” section for tips& strategies and also check out our “your questions answered” section where we answer your questions or send me an email to [email protected] with your questions!
Sincerely, your Friend
Patrik Hutzel
Related articles:
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- How long does it take to wake up from a Traumatic brain injury or severe head injury?
- What you need to do if your loved one in Intensive Care is brain dead or is considered for organ donation
- What is an induced coma and why is my critically ill loved one in an induced coma?
- How long can a breathing tube or an endotracheal tube can stay in?
- How long should a Patient be on a ventilator before having a Tracheostomy?
- Why does my loved one need a Tracheostomy in Intensive Care?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- Be more selfish if your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 4 ways on how to be more persuasive if your loved one is critically ill in Intensive Care
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


