Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED“ and in last week’s episode I answered another question from our readers and the question was
My Brother is in ICU Ventilated. Why Are They Covering the Worst-Case Scenario for my Brother?
You can check out last week’s question by clicking on the link here.
This is another episode of your questions answered and in today’s episode, I want to update you with a question that we’ve had from a client in the last couple of days. And the question is my 47-year old dad is in ICU with COVID-19 and he’s on a ventilator and the ICU team is telling me that he’s dying. Is this real?
My Dad is Ventilated in ICU with COVID-19. Is it True that He is Dying?

So this is really a timely episode. You know, it is now April 2020. And here at intensivecarehotline.com, we are very concerned about what we’re seeing all around the world, really our phones keep ringing all the time, with more and more patients going into ICU and into hospitals because of the coronavirus and the COVID-19 situation, again, all around the world. This is very concerning. Intensive care units all around the world seem to be getting more and more COVID-19 admissions, and more and more families are being locked out of intensive care because of precautions because of ICU’s obviously being concerned that a families get infected or be bringing in the virus themselves.
RECOMMENDED:
So this is a really grave situation, especially in the United States at the moment, in the UK very, very difficult situations and a lot of patients are unfortunately dying. And people and families can’t be with their loved ones. And this is a real tragedy all around the world unfolding at the moment. And also, it’s a tragedy for intensive care staff that is at high risk looking after coronavirus or COVID-19 patients, it’s equally important for intensive care staff to protect themselves from the virus.
So it’s an unprecedented situation that we’re seeing at the moment all across the world, whether it’s for patients, for families, and of course for the hard-working intensive care staff, caring for those patients.
RECOMMENDED:
But anyway, coming to our client, Jessica, that contacted us in the last few days, or in the last 48 hours even. She said that her dad has had symptoms since last Sunday of cough a fever, tiredness, fatigue.
And, you know initially, on Monday then he got tested for COVID-19 it obviously took about 48 hours to get the result back. After about 48 hours, the result came back as positive and within another less than 12 hours he ended up in the emergency room, struggling to breathe. He got admitted into intensive care initially he was breathing on BiPAP/CPAP. And then within less than another 12 hours he got intubated and ended up on a ventilator in an induced coma.
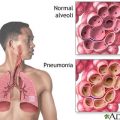
So when he first went into intensive care, they did a chest x-ray. It showed that his lungs had collapsed. He was developing more and more a picture of ARDS or lung failure, which again has COVID-19 patients get diagnosed with especially the ones that end up in ICU. Within hours, his kidneys shut down. He went into liver failure and showed signs of severe sepsis with significant hypotension blood pressure was dropping. He ended up on significant levels of inotropes and vasopressors.
RECOMMENDED:
And his heart, you know, seems to be still pretty strong. He’s got a normal heart rate of 80 to 100. His troponin was negative, so there was no sign of a heart attack or myocardial infarct. And the intensive care team couldn’t feed Jessica’s dad because he was just simply too sick to take any nutrients in. We have been talking to the doctors and the nurses to get a picture of what is happening.
Initially, when Jessica’s dad got intubated, he ended up on 100% of oxygen, or 100% of fio2 with a high co2 high carbon dioxide ended up on bicarbonate drip on a bicarbonate drip to manage the acidosis that resulted from the high co2.
He ended up in an induced coma, sedated with midazolam or versed and a little bit of fentanyl, which was stopped in the end because Jessica’s dad now is in a natural coma. He then ended up on Levophed at 30 micrograms an hour, epinephrine at 20 and vasopressin at 0.04. The pretty dire situation there and what happens with a lot of patients with ARDS, you can at least prone them, basically put them on their tummy to drain any excess fluids off the lungs and also to basically inflate or try to inflate the lungs by just turning a patient on their tummy head down.
RECOMMENDED:
But again, Jessica’s dad is too unstable to get prone at the moment, which really, you know, doesn’t help his situation. His inflammation markers are through the roof, his lactate is through the roof. Those are all signs of a very critical condition. He’s also on antibiotics even though he has been diagnosed with COVID-19.
The question that we had for the intensive care team was pretty much, what about referring him to an ECMO center? Because ECMO could potentially be life-saving or can be life-saving in a situation like that. I guess with his low blood pressure, and with significant amounts of inotropes or vasopressors, he’s probably too unstable to be transferred to an ECMO center. Because in the ICU where our client is, there is no ECMO available and they’re far away from the next at least two hours away from an ECMO center.
So the condition is really critical. And, you know, as I said, lung failure, ARDS, kidney failure and liver failure. And it looks like Jessica’s dad is, unfortunately, approaching his end of life fairly fast, which is really sad. He’s only 47 as I mentioned earlier and it’s really a stark warning for everyone that’s out there. And that social distancing is really important. Because you know, even young people are impacted by this severe pandemic situation at the moment.
RECOMMENDED:
It also goes to show that what we always say here at intensivecarehotline.com. If you have a loved one in intensive care, you need to think two steps ahead. You know, even when Jessica’s dad got admitted into ICU, they should have started their own research because again, most COVID-19 patients that end up in ICU end up with ARDS or lung failure from what I have read through my research and what I hear from other ICU professionals.
And when this is happening, you need to think ahead, because again, ECMO might have been an option even a couple of days ago, and the referral to an ECMO center might have been made a couple of days ago. This is what I always say. You don’t know what you don’t know. And if you don’t know what to look for and if you don’t know what questions to ask if you have a loved one in intensive care, you are fighting an uphill battle.
RECOMMENDED:
- YOU DON’T KNOW WHAT YOU DON’T KNOW WHEN YOUR LOVED ONE IS CRITICALLY ILL IN INTENSIVE CARE! (PART 1)
- YOU DON’T KNOW WHAT YOU DON’T KNOW WHEN YOUR LOVED ONE IS CRITICALLY ILL IN INTENSIVE CARE! (PART 2)
And you need to be prepared for all eventualities, the stakes are very high when you have a loved one in intensive care. And if you don’t know about treatment options, if you don’t know about the steps ahead, it’s very difficult for you to manage the dynamics. Intensive care team often is not sharing all treatment options with you unless you ask and especially at the moment where ICU’s are full and where ICU’s are operating at capacity.
You know, doctors and nurses are at their limits. So if you are not stipulating them with the right questions. It could be too late and it looks like for patients with Covid-19, they are deteriorating rapidly. And as you can see this situation where didn’t even take 48 hours for an otherwise fit and healthy 47-year-old man to go into multi-organ failure basically. And that might have been prevented if the right referral had been made maybe to another ICU early on, to have ECMO as a treatment option, Jessica and her family might have been prevented this situation.
RECOMMENDED:
So as I said, very dire situation out there in the world at the moment, unprecedented. I haven’t seen anything like it. I don’t think anybody living at the moment has anything like it, seen like it unless people have been through “World War II” or through “The Great Depression”. So we are living in unprecedented times at the moment and I can only urge everyone out there to keep managing this social distancing and help stop spreading this virus until it can hopefully be slowed down or a vaccine can be found.
So if you have a loved one in intensive care with COVID-19, or with any other critical illness, please contact us on one of the numbers on the top of the website or send me an email to support@intensivecare hotline.com. You see, this is another issue at the moment with so many COVID-19 patients in ICU.
RECOMMENDED:
Other admissions going into ICU may end up with COVID-19 or because of the infection risk or other issues, elective surgery gets canceled. And you know, other treatments for cancer patients or anybody else who needs an ICU bed or a hospital bed is at high risk or may not even get admitted at the moment.
So we’re really seeing again an unprecedented situation and again if you have a loved one in intensive care contact us.
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to you and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog“ section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!
Related Articles:
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care