Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question was
You can check out last week’s question by clicking on the link here.
In this episode of “YOUR QUESTIONS ANSWERED” I want to answer a question from one of my clients Joan as part of my 1:1 consulting and advocacy service! Joan’s dad is in ICU and is not as responsive as before. Joan is asking if her dad is being sedated by the medication that the ICU team is giving him.
My Dad is Less Responsive in ICU. Is He Being Sedated By The Medication that the ICU Team Is Giving Him?

Dear Patrik,
I tried to make this short but could not. I did leave a lot out, however.
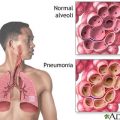
It is two months after my 71-year-old father had a stroke. He was in ICU for about two weeks after a procedure for decompression, and he has been ventilated and with an NG feeding tube ever since. He contracted pneumonia twice and another infectious disease.
RECOMMENDED:
He had a tracheostomy. The ICU unit had to be cleared because everybody on the floor contracted the same infection (antibiotic resistant, but dormant). He spent about two weeks in the infectious disease unit which was similar to the ICU.
He slept a lot, and was unresponsive a lot, but then he would wake up and could understand everything and seemed like the same person. He could follow all commands, and he put up a big struggle when the NG tube needed to be re-adjusted.
He was expressive and understood everything, even though he couldn’t talk or sit or anything like that. He was very weak from fighting off the infections, the antibiotics, the pneumonias, fever, etc.
After one month he went two days without a fever and was transferred to a geriatric center to the unit that specializes in respiratory rehabilitation. This place has an excellent reputation and good success with respiratory rehabilitation. There is a stroke rehabilitation unit in this same center however he was not transferred there.
The ride in the ambulance took a toll on him, and he arrived with a fever that lasted quite a while. And he was given more antibiotics. Finally when the fever went away, they began to work on his breathing.
That is the background, my current concern as of the last 2-3 weeks is that he seems much less alert and responsive now to me than he did before. He is not responsive most of the time, at least not when I am there. He is put in a chair.
There are days where he breathes on his own for about 12 hours at a time – which looks very painful, by the way. Cognitively he seems to be doing much worse to me than before and also at least one doctor at this center gave him a very low score in comparison to the assessment they gave him in the hospital. At first I was told it was the fatigue from breathing and the fever and all these other things.
But could it be the medications that they started giving him when he arrived here?
I spoke to a relative who is a neurosurgeon and he says he needs a CT to determine if something has changed, but they do not offer that at this center and his other family members are against transferring him. They are on a different branch of the family than the neurosurgeon.
When he was in the hospital before, he did contract multiple dangerous infections. And the ambulance ride was hard on him. For now, I would rather ask if the medications might be the culprit.
So finally, let me get to my point.
The doctors reluctantly agreed to remove Depalept 500mg 2x a day after being very dismissive about this request. This was about 10 days ago. However, it turns out they did not remove it. They only told us they did and today his wife confronted them about it.
So now they have said they will remove the Depalept against their own judgment and they will reduce the dose by half for the first 2 days and then stop it completely after another 2 days.
I am concerned that this is a very quick taper, 4 days when he has now been taking Depalept for almost a month since October 26th. At first they gave him 300mg 2x a day, then they upped the dose.
Also as you can see, the communication with the doctors at the center with our family is not the best. And also, I am clashing with family members as well about how to approach things.
However, one thing that my family members and I agree on is that the medications might be sedating him, and the biggest concern is this Depalept. And now, if the doctors really do remove the Depalept this time. I am very worried about this short 4-day schedule. Isn’t it important to taper off more slowly?
In the hospital, where he was for the first month, I don’t think they gave him any medications other than the antibiotics. I will find out for sure.
They said they gave him Depalept to stop his trembling according to other family members. I did not hear it from them myself. If that’s true, I don’t understand why that would matter in this situation. They did not say it was to prevent seizures or anything like that, though I do want to speak to them myself about this.
Thank you again sincerely, and wishing you a great day.
Regards,
Joan
RECOMMENDED:
Hello Joan,
Thank you Joan.
Is there a history of seizures?
Kind regards
Patrik
Hi Patrik,
Thank you for your reply.
No. He had a mini stroke a few years ago which left no effects and otherwise seemed very healthy, though he never went to the doctor.
Regards,
Joan
Hi Joan,
If there is no history of seizures, he shouldn’t be on Depalept in the first place. This is from Wikipedia here:
“Valproate (VPA), and its valproic acid, sodium valproate, and valproate semi sodium forms, are medications primarily used to treat epilepsy and bipolar disorder and to prevent migraine headaches.
They are useful for the prevention of seizures in those with absence seizures, partial seizures, and generalized seizures. They can be given intravenously or by mouth. Long and short acting formulations of tablets exist.
Common side effects include nausea, vomiting, sleepiness, and dry mouth. Serious side effects can include liver problems and regular monitoring of liver function tests is therefore recommended. Other serious risks include pancreatitis and an increased suicide risk. The drug is known to cause serious abnormalities in babies if taken during pregnancy. Because of this it is not typically recommended in women of childbearing age who have migraines.
My experience from Depalept is to only use it for seizure/epilepsy management.
I couldn’t find any reliable literature about the weaning time for Depalept, it suggests that weaning off Depalept when having seizures could be an issue. Given that your Dad has no history of seizures the Depalept is just sedating him that’s all. Therefore the sooner he can be liberated the better.
Does that make sense?
KInd Regards
Patrik
Dear Patrik,
Yes this make sense. I wondered if having a stroke is in itself a risk factor for seizures? However, they only said it was to stop the trembling. And again, he has never had a seizure.
Thank you so much. It unfortunately turned into a kind of conflict with one of the doctors who said he had all these years of experience and here we are telling him what to do. So your input is reassuring and helpful. I was there a few hours ago and saw that they have reduced the dose to 250mg twice a day for now.
I won’t be too concerned if he starts to tremble again. What I care about is figuring out why his awareness level has changed so much, why he isn’t able to follow instructions like before etc.
Thank you again and best regards,
Joan
Hello Joan,
How are you? I hope everything will turn out fine for you and your dad.
Anyway, with regards to your last email:
Joan: I wondered if having a stroke is in itself a risk factor for seizures? However, they only said it was to stop the trembling. And again, he has never had a seizure.
When was the last time they did a CT scan or Brain MRI for your dad? It is important for your dad to undergo such a procedure to determine what is the current status of the part of the brain that has been affected and what really causes the trembling. And if they are telling that it is not seizure, then what could it be and that she has to be started with Depalept?
Here are a few good points from reliable sources:
NICE (National Institute for Health Care and Excellence) guidelines suggest to consider AED (anti-epileptic drugs) for a patient after a first unprovoked seizure if the patient has a neurological deficit or abnormality on brain imaging, which could be said to apply to stroke patients.
Post?stroke seizure and post?stroke epilepsy are common causes of hospital admissions, either as a presenting feature or as a complication after a stroke.
They require appropriate management and support in long term.
Joan: It unfortunately turned into a kind of conflict with one of the doctors who said he had all these years of experience and here we’re telling him what to do. So your input is reassuring and helpful. I was there a few hours ago and saw that they have reduced the dose to 250mg twice a day for now.
Conflicts among relatives of the patients in the ICU with the doctors are common especially if the relatives are knowledgeable with what is happening to their loved one. It is a form of self-defense for them I may say.
But after you said your point which really makes sense with the current appropriate management for your dad, later on, the doctor for sure would realize that and do research too as well on his own. They may be experienced doctors, yes, but the appropriate care and management for specific diagnosis especially for the case of your dad has significant improvements to aid in their recovery. And the way you communicate to them and share your point is important too.
Based on the best available evidence, we would recommend treating the initial seizure post-stroke if it occurs more than seven days after the event. We would suggest, after careful discussion with the patient or relatives about the risks and intended benefits of AED (anti-epileptic drug) therapy, treating with an appropriate first-line AED, such as lamotrigine or sodium valproate, for at least 1 year before considering tapering the dose.
Joan: I won’t be too concerned if he starts to tremble again. What I care about is figuring out why his awareness level has changed so much, why he isn’t able to follow instructions like before etc.
What are his current medications? Depalept can cause sleepiness, other medications will do too as well. If your dad continued to have this trembling, I would be alarmed as to what might cause it. We need to rule it out and give your dad the necessary treatment and medication to control or totally eliminate it.
Is the ICU team informing you about your dad’s Glasgow Coma Scale (GCS)? GCS is a neurological scoring system used to assess conscious level. What is your dad’s current GCS score? How frequent are they assessing it? Any EEG? We need to gather these data.
I hope this helps.
For any questions still, please let us know.
Kind regards,
Patrik
RECOMMENDED:
Dear Patrik,
Thank you for your incredibly helpful response.
I have scheduled an appointment to speak with the prescribing physician tomorrow and will be much better prepared with what to ask him now Patrik. I will ask him about the factors discussed in the article that you sent me thank you so very much.
My father has not had any CT scan or Brain MRI since about a week before he left the hospital, so probably not since the first week of October. They do not offer them at this rehabilitation center. He would have to be transported back to the hospital to have this done.
The relatives who have guardianship are opposed to this option. I am going to contact my neurosurgeon relative to ask about something he mentioned, a portable CT scan.
The doctor that prescribed the Depalept actually said that if the family wanted them to stop it, they would do so right away. The conflict came about with the head of the department, who is renowned for his success in respiratory rehabilitation.
However, by the way, his respiration has improved greatly in the last couple of days though his eyes are closed almost all the time. Yes, communicating with doctors properly is a delicate issue.
Tomorrow when I talk to the doctor I will ask about my father’s current GCS. From mid-October when he left the hospital I have the following I don’t know if it’s his GCS.
Eye Opening: 4 – Spontaneous
Verbal Response: 1 – None (he could not talk with the tracheostomy tube, but he did try).
Motor Response: 6- Obeys Commands
Score: 11
What are his current medications?
This is a very important question. I have the list. I will send separately.
Happy Holidays and many, many thanks again!!!
Regards,
Joan
RECOMMENDED:
Hello Joan,
We are indeed grateful that we are able to help you and your dad.
Anyway, thank you for your response and will wait for additional clinical information from you.
Happy Holidays to you and to your family!
Regards,
Patrik
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to Eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to you and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!