What are seizures?
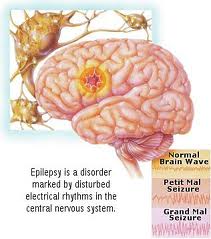
An epileptic seizure, sometimes referred to as a fit, is defined as a transient symptom of “abnormal excessive or synchronous neuronal activity in the brain”. In other words, normal brain activity is suddenly disturbed as electrical activity has spread uncontrollably from one part of the brain to the other part of the brain. The outward effect can be as dramatic as a wild thrashing movement (tonic-clonic seizure) or as mild as a brief loss of awareness (absence seizure). It can manifest as an alteration in mental state, tonic or clonic movements, convulsions, and various other psychic symptoms (such as déjà vu or jamais vu). Sometimes it is not accompanied by convulsions but a full body “slump”, where the person simply will lose body control and slump to the ground. During a seizure, normal brain function such as memory, awareness of surrounding, consciousness, movement etc… is temporarily lost. The medical syndrome of recurrent, unprovoked seizures is termed epilepsy, but seizures can occur in people who do not have epilepsy.
About 4% of people will have an unprovoked seizure by the age of 80 and the chance of experiencing a second seizure is between 30% and 50%.Treatment may reduce the chance of a second one by as much as half.Most single episode seizures are managed by primary care physicians (emergency or general practitioners), whereas investigation and management of ongoing epilepsy is usually done by neurologists.
- What causes seizures?
- What are the different types of seizures?
- What is the treatment?
- What happens in Intensive Care?
- How long will the Patient remain in Intensive Care?
What causes seizures?
- Epilepsy
- Stroke
- Head injury
- Brain tumour
- Infection (meningitis, abscess)
- Drug abuse and overdoses
- Low salt levels in the blood(hyponatremia)
- Low blood sugar (hypoglycemia)
- Fever (in children)
- Alcohol or drug withdrawal
- dehydration
- sleep deprivation
- Arteriovenous malformation (AVM)
- normal doses of certain drugs that lower the seizure threshold, such as tricyclic antidepressants
- Encephalitis, Meningitis
- fever leading to febrile convulsions
- hypoxia(lack of oxygen)
- seizures in a person with hydrocephalus may indicate severe shunt failure
- PTSD(Post traumatic stress disorder)
Following extensive testing, a first seizure may later be diagnosed as epilepsy. About 50% of the people who have a seizure without any diagnosed cause will go on to have another seizure. There is a very high likelihood to have another seizure after the first one, if a person has had a brain injury or a previous abnormality. If someone has already had two seizures, there is an 80% chance that more will occur.
Prolonged and recurrent seizures in a person with known epilepsy are usually caused by failing to take prescribed drugs to stop seizures, change to the dose or medication used to control seizures, or alcohol withdrawal.
What are the different types of seizures?
- Partial seizures (also called focal seizures and localized seizures) are seizures which affect only a part of the brain at onset. In partial seizures a small part of one of the lobes may be affected and the person remains conscious. This will often be a precursor to a larger seizure such as a complex partial seizure. This type of seizure may cause twitching of one limb, or unusual tastes or sensations such as pins and needles in a specific part of the body
- A complex partial seizure is an epileptic seizure that is associated with bilateral cerebral hemisphere involvement and causes impairment of awareness or responsiveness, i.e. alteration of consciousness and the person has limited or no memory of what happened. These seizures will also be characterised by apparent confusion and automatic movements(such as fiddling with clothes, chewing, or wandering about). The person may respond if spoken to. The seizure might also occur as a visual disturbance, such as tunnel vision or a change in the size of objects. Once consciousness is impaired, the person may display automatism’s such as lip smacking, chewing or swallowing. There may also be loss of memory (amnesia) surrounding the seizure event. The person may still be able to perform routine tasks such as walking. Witnesses may not recognize that anything is wrong
- Generalised seizures, as opposed to partial seizures, are a type of seizure that impairs consciousness and distorts the electrical activity of the whole or a larger portion of the brain (which can be seen, for example, on Electroencephalograph (EEG) and the person is loosing consciousness. Generalised epilepsy is primary because the epilepsy is the originally diagnosed condition itself, as opposed to secondary epilepsy, which occurs as a symptom of a known as diagnosed condition. Generalised seizures often occur with no pre- warning and memory is lost. Grand mal seizure or tonic clonic convulsive seizure is the most common manifestation of the Generalised seizure. Initially, the person affected by the seizure collapses on the floor, bite their tongue or cry out. The muscles start to spasm(relax and tighten). Breathing usually is difficult and the person might lose control of bladder and bowel movement. After the seizure, the person might feel tired, confused, and has a headache
- In tonic seizures, there is general stiffening of the muscles without any jerking. The person might fall to the ground and may hurt themselves, but recovery is generally quick.
- Atonic seizures are a type of seizure that consist of a brief lapse in muscle tone that are caused by temporary alterations in brain function. The seizures are brief – usually less than fifteen seconds are very uncommon, and involve sudden loss of muscle tone causing the person to fall (drop attacks). The person might be injured by the fall, but recovery is generally rapid. Atonic seizures can occur while standing, walking or sitting, and are often noticeable by a head drop (the neck muscles releasing) and damage sometimes results from hitting the face or head. As with common epileptic occurrences, no first aid is needed post-seizure, except in the instances where falling injuries have occurred. In some cases, a person may become temporarily paralyzed in part of his or her body. This usually does not last longer than 3 minutes.
- Myoclonic seizures involve brief and abrupt jerking of one or more limbs. This can occur by itself, or with generalised seizures, shortly before the person wakes up
- Absence seizures are sometimes referred to as petit mal seizures(from the French for “little illness”, a term dating from the late 18th century). Absence seizures are brief (usually less than 20 seconds), generalized epileptic seizures of sudden onset and termination, mainly in children. They have two essential components, with the impairment of consciousness (absence) and the Electroencephalograph (EEG) shows generalized spike-and-slow wave discharges. The person affected experiences a brief interruption of consciousness and becomes unresponsive for several seconds. They may appear blank or staring usually without any other features, except perhaps for a fluttering of the eyelids.
What is the treatment for seizures in the Intensive Care Unit?
Seizure activity must be stopped promptly, and numerous drugs can be given to do this. If your loved one is in the Intensive Care unit and has seizures, drugs that stop seizures are given through an intravenous cannula, sometimes as a continuous infusion (such as Midazolam, Diazepam, Lorazepam, Clonazepam, Propofol or Phenytoin). It is important to put the Patient in a position to ensure safety and to prevent them from harming themselves. Oxygen may be administered, and in severe cases, especially where the person has sever breathing difficulties, the Patient may need to be intubated(Intubation) and mechanically ventilated with Ventilators (Breathing Machines).
Potentially sharp or dangerous objects should also be moved from the vicinity, so that the individual is not hurt. After the seizure if the person is not fully conscious and alert, they should be placed in the recovery position.
Ongoing medication is not typically needed after a first seizure and is generally only recommended after a second seizure has occurred. However, in severe cases where Patients experience frequent unpredictable seizures everyday, the use of anti-epileptic drugs (AEDs) are recommended to reduce the likelihood and duration of seizures. Approximately 70% of the Patients could have the seizures fully under control with continuous use of medication

What happens in the Intensive Care Unit?
- Your loved one is continuously monitored with a Bedside Monitors– Your loved ones vital signs such as Blood pressure is usually displayed continuously on the bedside monitor via an Arterial Catheter. Your loved ones Heart, Heart rhythm(ECG), temperature and breathing rate is continuously monitored and displayed on the monitor. Oxygen levels are continuously monitored by an oxygen saturation probe attached to the finger or to the ear. Furthermore oxygen levels are intermittently checked with ABG’s(Arterial Blood Gases), where blood is drawn out of the Arterial Catheter and tested immediately via a Blood Gas Analyser.
- Your loved ones breathing will be supported by additional oxygen via an oxygen mask, or Non- Invasive Ventilation(NIV) or BIPAP ventilation, however your loved one may be on a Ventilator (Breathing Machine) and have a Breathing Tube (Endotracheal tube) inserted into their airway. Some Patients affected by seizures are in an induced Coma and therefore require mechanical ventilation with a Ventilator (Breathing Machine).
- If your loved one has a head or brain injury they may require Intracranial Pressure Monitoring, which basically monitors the pressure in your loved ones head
- Your loved one will be receiving intravenous fluids via several intravenous cannula’s or Central Venous Lines(central line or CVC). This may include sedatives to prevent and control seizures and can also be used for Ventilator tolerance
- A Urinary Catheter is used to monitor urine output and a Nasogastric Tubes will be used to rest the intestine if this has been injured or if your loved one requires ventilation.
- You can expect your loved one to have frequent Chest X-rays and blood tests(Blood& Pathology tests in Intensive Care) especially arterial blood gases (ABGs)
- Sometimes an EEG – Electroencephalography is done, if it is unclear whether your loved one has actually had, or is still having a seizure.
- Other tests might be used to look for possible causes for the seizures, such as a head CT scan, or lumbar puncture (to take a sample of spinal fluid to exclude infection).
How long will your loved one remain in Intensive Care?
Your loved one will remain in intensive care while they have investigations and treatment. If they continue to require an endotracheal tube and ventilator, they will continue to be managed in the ICU. Each patient’s condition is very unique and it is important to speak with the medical team caring for the patient to discuss the potential outcome and prognosis.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
Related Articles:
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- How long does it take to wake up from a Traumatic brain injury or severe head injury?
- What you need to do if your loved one in Intensive Care is brain dead or is considered for organ donation
- How long can a breathing tube or an endotracheal tube can stay in?
- How long should a Patient be on a ventilator before having a Tracheostomy?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Why does my loved one need a Tracheostomy in Intensive Care?
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- Be more selfish if your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 4 ways on how to be more persuasive if your loved one is critically ill in Intensive Care
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- How long does it take to wake up from a Traumatic brain injury or severe head injury
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure