Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Loved ones in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question was
My Mom is Brain Dead in ICU. Do They Want to “Pull the Plug” Because of Organ Donation?
You can check out last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer questions that we get quite frequently as part of my 1:1 consulting and advocacy service!
HOW TO ASSESS GLASGOW COMA SCALE (GCS) IN ADULTS AND CHILDREN?

The Glasgow Coma Scale (GCS) is a neurological evaluation tool that allows healthcare professionals to consistently evaluate the consciousness level of your loved one. It is commonly used in the context of head trauma, but it is also useful in a wide variety of other non-trauma related settings.
In the case when your loved one is given medications intended to put them into an induced coma, it is also important to monitor their Glasgow coma scale to be able to know if there is already an overdose of medications because it can be equally lethal. Monitoring of the Glasgow coma scale serves as a guide to determine if the targeted level of an induced coma is achieved or thus need to be increased or tapered down depending on the result of your loved one’s GCS scoring.
By regularly assessing a loved one’s GCS, a downward trend in consciousness level can be recognized early, allowing time for appropriate interventions to be performed. 1
The Glasgow Coma Scale is the most used tool in hospital and pre-hospital environments. Some of the advantages of the GCS is that it’s easy to use and it facilitates a common language and objective. That, in turn, makes communication between healthcare professionals much easier.
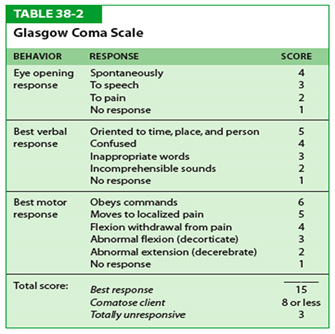
There are three aspects of behavior that are independently measured as part of an assessment of your loved one’s GCS – eye-opening, verbal performance and motor responsiveness. The highest response from each category elicited by the healthcare professional is scored on the chart.
When applying the GCS, the final score is determined by adding the values of E + V + M (eye opening score + verbal response score + motor response score). This number helps medical practitioners categorize the possible levels for survival, with a lower number indicating a more severe injury and a poorer prognosis. Following is a breakdown of the scoring:
- mild brain injury —a score of 13 to 15
- moderate brain injury—a score of 9 to 12 (this usually suggests that there was a loss of consciousness greater than 30 minutes.)
- severe brain injury is a score of 3 to 8
* The highest possible score is 15 (fully conscious) and the lowest possible score is 3 (coma or dead).
Eight is considered a critical score with 90 percent of loved ones in a coma at this level or below. A coma is defined as:
- not opening eyes
- not obeying commands
- not uttering understandable words
3 ELEMENTS OF THE GLASGOW COMA SCALE
EYE RESPONSE (E)
A maximum possible score of 4 points

Eyes opening spontaneously (4 points)
To assess eye response, initially observe the loved one for spontaneous eye-opening. If the loved one is opening their eyes spontaneously, your assessment of this behavior is complete, with the loved one scoring 4 points. You would then move on to assessing verbal response, as shown in the next section.
If however, the loved one is not opening their eyes spontaneously, you need to work through the following steps until a response is obtained.
Eyes opening to speech (3 points)
If your loved one doesn’t open their eyes spontaneously, you need to speak to your loved one “Hey Miss Smith, are you ok?” If the loved one’s eyes open in response to the sound of your voice, they would score 3 points.
Eyes opening to pain (2 points)
If your loved one doesn’t open their eyes in response to sound, you need to move on to assessing eye-opening to pain. If the loved one’s eyes open in response to a painful stimulus, they would score 2 points.
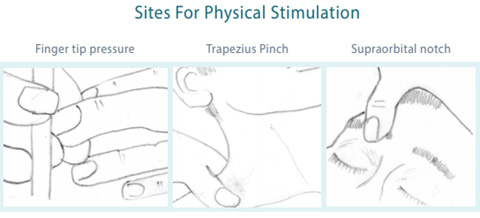
There are different ways of assessing response to pain, but the most common are:
- Applying pressure to one of the fingertips
- Squeezing one of the trapezius muscles (referred to as a “trapezius squeeze”)
- Applying pressure to the supraorbital notch
No response (1 point)
If your loved one does not open their eyes to a painful stimulus, they score 1 point.
Not testable (NT)
If the loved one cannot open their eyes due to edema, trauma, dressing etc, you should document that eye response could not be assessed (NT).
VERBAL RESPONSE (V)
A maximum possible score of 5 points
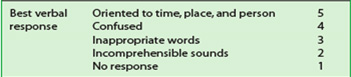
Assessing a loved one’s verbal response initially involves trying to engage the loved one in a conversation and assess if they are orientated. You should score the loved one based on the highest scoring response they demonstrate during the assessment.
Some common questions you can ask to help assess this might include:
- “Can you tell me your name?”
- “Do you know where you are at the moment?”
- “Do you know what the date is today?”
Orientated response (5 points)
If your loved one is able to answer your questions appropriately, the assessment of verbal response is complete, with the loved one scoring 5 points.
Confused conversation (4 points)
If your loved one is able to reply, but their responses don’t seem quite right (e.g. they don’t know where they are, or what the date is), this would be classed as confused conversation and they would score 4 points. Sometimes confusion can be quite subtle, so pay close attention to their responses.
Inappropriate words (3 points)
If your loved one responds with seemingly random words that are completely unrelated to the question you asked, this would be classed as inappropriate words and they would score 3 points.
Incomprehensible sounds (2 points)
If your loved one is making sounds, rather than speaking words (e.g. groans) then this would be classed as incomprehensible sounds, with the loved one scoring 2 points.
No response (1 point)
If your loved one has no response to your questions, they would score 1 point. If your loved one is intubated or with tracheostomy, or has other factors interfering with their ability to communicate verbally, you would also score 1.
MOTOR RESPONSE (M)
A maximum possible score of 6 points
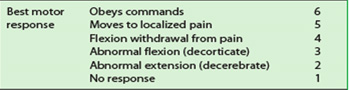
The final part of the GCS assessment involves assessing a loved one’s motor response.
You should score your loved one based on the highest scoring response you were able to elicit in any single limb (e.g. if they were unable to move their right arm, but able to obey commands with their left arm, they’d receive a score of 6 points).
Obeys commands (6 points)
Ask the loved one to perform a two-part request (e.g. “Lift your right arm off the bed and make a fist.”). If they are able to follow this command correctly, they would score 6 points and the assessment would be over.
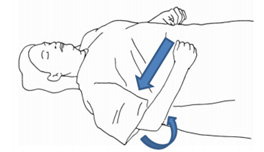
Localises to pain (5 points)
This assessment involves you applying a painful stimulus and observing the loved one for a response.
There are different ways of assessing response to pain, but the most common are:
- Squeezing one of the loved one’s trapezius muscles (referred to as a “trapezius squeeze”)
- Applying pressure to the loved one’s supraorbital notch
 If your loved one makes attempts to reach towards the site at which you are applying a painful stimulus (head/neck) and brings their hand above their clavicle, this would be classed as localising to pain, with the loved one scoring 5 points.
If your loved one makes attempts to reach towards the site at which you are applying a painful stimulus (head/neck) and brings their hand above their clavicle, this would be classed as localising to pain, with the loved one scoring 5 points.
Withdraws to pain (4 points)
 This is another possible response to a painful stimulus, which involves your loved one trying to withdraw from the pain (e.g. the loved one tries to pull their arm away from you when applying a painful stimulus to their fingertip). This response is also referred to as a “normal flexion response” as the loved one typically flexes their arm rapidly at their elbow to move away from the painful stimulus.
This is another possible response to a painful stimulus, which involves your loved one trying to withdraw from the pain (e.g. the loved one tries to pull their arm away from you when applying a painful stimulus to their fingertip). This response is also referred to as a “normal flexion response” as the loved one typically flexes their arm rapidly at their elbow to move away from the painful stimulus.
It differs from the “abnormal flexion response to pain” shown below due to the absence of the other features mentioned (e.g. internal rotation of the shoulder, pronation of forearm, wrist flexion). Withdrawal to pain scores 4 points on the Glasgow Coma Scale.
Abnormal flexion response to pain (3 points)
Abnormal flexion to a painful stimulus typically involves adduction of arm, internal rotation of the shoulder, pronation of forearm and wrist flexion (known as decorticate posturing).
Decorticate posturing indicates that there may be significant damage to areas including the cerebral hemispheres, the internal capsule, and the thalamus.
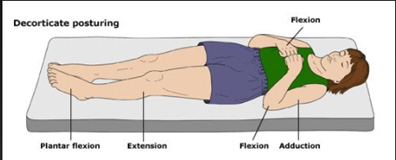
What causes decorticate posture?
- an intracranial hemorrhage (bleeding in the brain)
- brain abscess
- primary or secondary brain tumor
Abnormal extension response to pain (2 points)
Abnormal extension to a painful stimulus is also known as decerebrate posturing. In decerebrate posturing, the head is extended, with the arms and legs also extended and internally rotated. The loved one appears rigid with their teeth clenched. The signs can be just one side of the body or on both sides, and it may just be in the upper limbs.
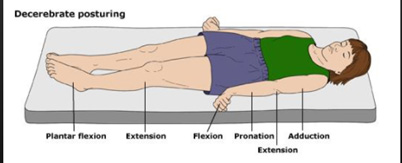
What causes decerebrate posture?
- stroke
- intracranial hemorrhage
- primary or secondary brain tumor
- encephalopathy or hepatic encephalopathy
- head injury
- increased intracranial pressure
- brain stem tumor
No response (1 point)
The complete absence of a motor response to a painful stimulus scores 1 point.
Not testable (NT)
If the loved one is unable to provide a motor response (e.g. paralysis), this should be documented as not testable (NT).
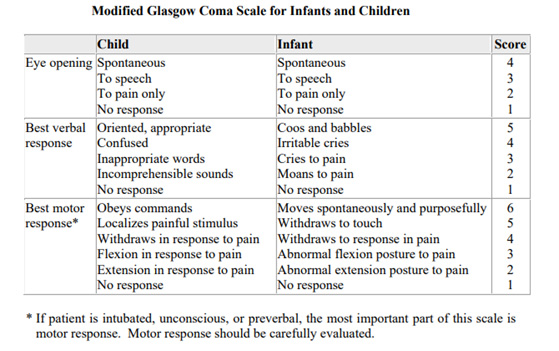
Understanding the Pediatric Glasgow Coma Scale

The Glasgow Coma Scale (GCS) is a widely used scoring system for quantifying the level of consciousness following traumatic brain injury. It is used because it is simple, has a relatively high degree of reliability and correlates well with outcomes following severe brain injury. One of the components of the scale is the “verbal response,” which cannot be assessed when children are very young. A modified version of the scale—the Pediatric Glasgow Coma Scale (PGCS)—was created for children too young to talk. 2
When it comes to health of your loved one, the more precise we can be with the terms and concepts that we use, the better. That’s why the Glasgow Coma Scale is so useful because it allows providers to avoid ambiguities like “the loved one is drowsy, unconscious, or comatose” especially if your loved one is in induced coma. We can also be more exact about the clinical state and evolution of the loved one. The Glasgow Coma Scale gives providers precision and certainty.
In addition, the precision and relative simplicity of this scale make it universally popular. Experts use it for other traumatic and non-traumatic pathologies. Professionals in diverse fields use it for emergency situations and a useful tool especially in ICU for loved ones on sedation and induced coma.
The GCS is a complete tool that evaluates three key aspects. The best part of all is that healthcare professionals can use it again and again. This scale offers longitudinal information about the evolution of a coma. Consequently, it’s very useful in the early stages of treatment.
REFERENCES:
- The Glasgow Coma Scale: Definition, Use, and Advantages
https://exploringyourmind.com/glasgow-coma-scale-definition-use-advantages/
- Understanding the Pediatric Glasgow Coma Scale
https://www.rainbowrehab.com/understanding-pediatric-glasgow-coma-scale/
- Glasgow Coma Scale
https://en.wikipedia.org/wiki/Glasgow_Coma_Scale#Eye_response_(E)
- Decerebrate image
https://s3.amazonaws.com/classconnection/550/flashcards/1323550/png/screen_shot_2015-02-24_at_53215_pm-14BBDEF3BE53973FC88.png
- Guidelines for Basic Adult Neurological Observation
https://www.criticalcareontario.ca/EN/Education/CCSO%20Webinar-Adult%20BNO%20Guidelines-Nov%2012%202015.pdf
- Glasgow Coma Scale (GCS)
https://geekymedics.com/glasgow-coma-scale-gcs/
- GLASGOW COMA SCALE : Do it this way: Institute of Neurological Sciences NHS Greater Glasgow and Clyde
https://www.glasgowcomascale.org/downloads/GCS-Assessment-Aid-English.pdf?v=3
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to you and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!







