What is intracranial pressure monitoring?
The monitoring of intracranial pressure(ICP monitoring) is used in treating severe Traumatic Brain Injury (TBI) Patients, but it can also be used after brain surgery. This process is called intracranial pressure monitoring(ICP monitoring). All current clinical available measurement methods are invasive and use various transducer systems (most used is insertion of a catheter into the cranium).
When the brain suffers fom severe trauma it begins to swell inside the skull. If the brain swelling goes undetected and is not treated, the brain becomes deprived of oxygen-rich blood and “starves”. This lack of oxygen causes permanent brain damage. With ICP Monitoring, which tells doctors and nurses how much swelling the brain has sustained and can drain cerebrospinal fluid, which would relieve some of the pressure, this outcome can be prevented.


How Does it Work?
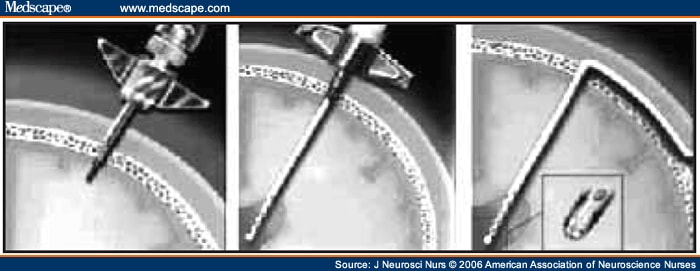
The specialised probe, measuring Intracranial pressure, is inserted into the brain using a small burr hole. This may happen during scheduled surgery or in the ICU. If the probe is only measuring the pressure within the skull it will be attached to the ‘intra-cranial pressure monitor’(ICP Monitor). This monitor may be a separate monitor or integrated as part of the Bedside Monitors.
If the probe is inserted into a ventricle of the brain there will also be a drainage system whereby CSF can be removed from the ventricles. CSF (cerebrospinal fluid) is a clear fluid surrounding the brain to cushion it from the hard skull.
When the pressure in the brain increases, doctors and nurses may alter your loved ones treatment depending on a number of factors. This may include the removal of small amounts of CSF, but it may also include more sedation, high concentrated Saline to reduce the brain swelling, to make more room in the skull for the brain and assist in reducing the pressure inside the skull.
How Long Will It Be Used For?
The ICP monitor or drain usually stays in place until the pressures in the brain have been stabilised and are under control. This may take a few days, but can also be longer, depending on your loved ones condition.
Are There Any Complications?
Complications that may occur infrequently are
- Intracranial infection
- Intracerebral hemorrhage(bleeding)
- Air leakage into the ventricle or subarachnoid space
- CSF leakage
- Overdrainage of CSF leading to ventricular collapse and herniation
- Loss of monitoring or drainage capabilities due to the occlusion of the catheter with brain tissue or blood
- Inappropriate therapy because of erroneous ICP readings due to dampened waveforms, electromechanical failure, or operator error(i.e. inappropriate leveling)
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual patient. Please refer to the full disclaimer.
Related articles:
-
How long does it take to wake up from a Traumatic brain injury or severe
head injury?
-
How to take control if your loved one has a severe brain injury and is
critically ill in Intensive Care
-
What is an induced coma and why is my critically ill loved one in an
induced coma?
-
The 3 most dangerous mistakes that you are making but you are unaware of,
if your loved one is a critically ill Patient in Intensive Care
-
How to always achieve your goals whilst your loved one is critically ill in
Intensive Care
-
Follow this proven 5 step process on how to be in control and influential if
your loved one is a long-term Patient in Intensive Care
-
How to quickly take control and have real power and influence if your loved
one is critically ill in Intensive Care
-
How long can a breathing tube or an endotracheal tube can stay in?
-
3 quick steps on how to position and prepare yourself well mentally, whilst
your loved one is critically ill in Intensive Care
-
How to get what you want whilst your loved one is critically ill in Intensive Care
-
5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
-
How to make sure that your values and beliefs are known whilst your loved one is
critically ill in Intensive Care
-
How to make sure that “what you see is always what you get” whilst your loved one is
critically ill in Intensive Care
-
What the doctors and the nurses behaviour in Intensive Care is telling you about
the culture in a unit
-
Family Meetings in Intensive Care or the Elephant in the Room
-
What you need to do if your loved one is dying in Intensive Care(part one)
-
What you need to do if your loved one is dying in Intensive Care(part two)
-
Intensive Care at its best?
-
How We Can Help You
-
What you and your Family need to do if your critically ill loved one is very sick in
Intensive Care and faces an uncertain future
-
How long should a Patient be on a ventilator before having a Tracheostomy?
-
How long can somebody stay in Intensive Care?
-
My Family can’t agree on what’s best for my sister in Intensive Care…Help!
-
My husband is dying in Intensive Care, but we need more time…
-
My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


