Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question was
You can check out last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer a question that we get quite frequently as part of my 1:1 consulting and advocacy service!

How Many Patients Die in Intensive Care (ICU)?
Mortality rates in the ICU (Intensive Care Unit) strongly depend on the severity of illness and the patient population analyzed. Admissions in the ICU vary in different countries. More than 5 million patients are admitted annually in United States, while there were 230,800 adult ICU admissions in Canada, an estimate of between 10,000 and 15,000 critically ill adult patients require critical care in ICUs each year in Ireland, ICU admissions each year in the United Kingdom of 271,079 with 160,000 patients admitted to Intensive Care Units (ICUs) in Australia and New Zealand and Germany, with 1.9 million ICU admissions annually.
The average mortality rate reported in the United States ranges from 8-19% or 500,000 deaths annually. Acute care separations that ended in death accounted only for 10% in Australia and New Zealand. ICU deaths occurring in Canada comprise 29.2% for one fiscal year, while there was an estimated 16,424 ICU mortality for the United Kingdom for the most recent year 2015 – 16. Please see table below:
| NHS Digital – Hospital Adult Critical Care Activity – 2015-16 Report
Breakdown of critical care unit discharge status1 |
||||
| 2014-154 | 2015-16 | |||
| Critical care unit discharge status | Number of critical care records | Percentage of critical care records | Number of critical care records | Percentage of critical care records |
| Fully ready for discharge | 100,863 | 57.1% | 103,243 | 55.9% |
| Delayed discharge due to shortage of other ward beds | 41,548 | 23.5% | 46,146 | 25.0% |
| Patient died (no organs donated) | 15,205 | 8.6% | 15,606 | 8.5% |
| Current level of care continuing in another location | 9,513 | 5.4% | 9,842 | 5.3% |
| More specialised care in another location | 3,962 | 2.2% | 4,303 | 2.3% |
| Early discharge due to shortage of critical care beds | 3,257 | 1.8% | 2,929 | 1.6% |
| Discharge for palliative care | 941 | 0.5% | 983 | 0.5% |
| Self discharge against medical advice | 507 | 0.3% | 705 | 0.4% |
| Patient died (heart beating solid organ donor) | 438 | 0.2% | 426 | 0.2% |
| Patient died (cadaveric tissue donor) | 290 | 0.2% | 259 | 0.1% |
| Patient died (non heart beating solid organ donor) | 115 | 0.1% | 133 | 0.1% |
| Sub total | 176,639 | 100.0% | 184,575 | 100.0% |
| Unknown / not recorded | 83,052 | 32.0% | 86,504 | 31.9% |
| Total | 259,691 | 100.0% | 271,079 | 100.0% |
One research study from Canada, hospital beds and adult ICU beds per 100,000 population internationally showed an overall unadjusted ICU mortality of 9% in Canada. Internationally, there is wide variation in mortality rates, from 6% in Germany and 10% in the U.S., to 29% in the U.K.
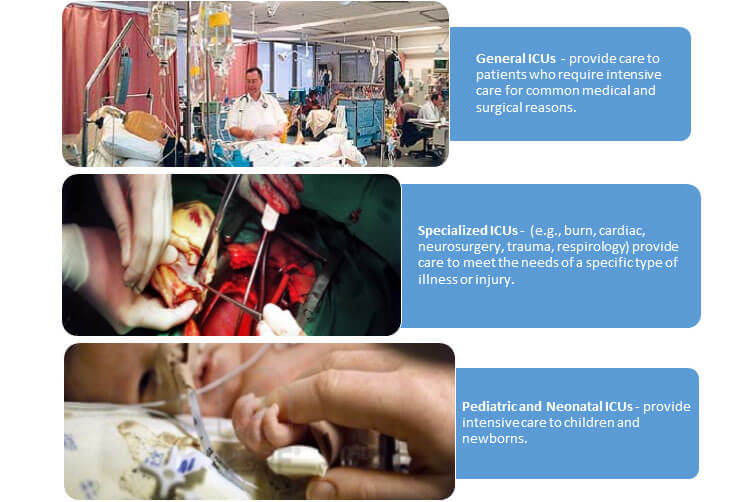
There are different types of ICUs that provide care to specific patient populations categorized as:
WHAT ARE THE REASONS FOR ADMISSION TO THE ICU?
- intensive or invasive monitoring
- support of airway, breathing or circulation
- stabilization of acute or life-threatening medical problems
- comprehensive management of injury and/or illness
- restoration to stable health status or comfort while dying within an interdisciplinary and collaborative environment.
The Intensive Care Unit (ICU) is the part of the hospital where care is provided to the sickest patients. It is typified by having a high level of monitoring and therapeutic technologies, a very high degree of organization and high staff to patient ratios.
Despite the high severity of illness of patients admitted to ICU, most improve to the point to be discharged to a normal ward care environment. A significant proportion of these ICU-discharged patients subsequently die in the hospital with post-ICU mortality rates ranging from 6 to 27% [1–7] either as a result of residual organ dysfunction/failure or due to the inability of the staff in lower levels of care to cope appropriately with the needs of these patients.
Although patients in intensive care units (ICUs) receive care for a large variety of disease states, the leading causes of death in the ICU are:
CARDIOVASCULAR FAILURE

Cardiovascular system failure is commonly faced by the intensivist. Heart failure can occur due to a host of predisposing cardiac disorders or as secondary effects of systemic illness. When the heart is unable to provide an adequate cardiac output to maintain adequate tissue perfusion, cardiogenic shock ensues. Without prompt diagnosis and appropriate management, these patients have significant morbidity and mortality, with in-hospital mortality approaching 60% for all age groups.
WHAT IS A CARDIOGENIC SHOCK?
Cardiogenic shock is a condition in which your heart suddenly can’t pump enough blood to meet your body’s needs. The condition is most often caused by a severe heart attack, but not everyone who has a heart attack has cardiogenic shock.
Cardiogenic shock is rare, but it’s often fatal if not treated immediately. If treated immediately, about half the people who develop the condition survive.
CARDIOGENIC SHOCK SIGNS AND SYMPTOMS:
- Rapid breathing
- Severe shortness of breath
- Sudden, rapid heartbeat (tachycardia)
- Loss of consciousness
- Weak pulse
- Low blood pressure (hypotension)
- Sweating
- Pale skin
- Cold hands or feet
- Urinating less than normal or not at all
SYMPTOMS OF A HEART ATTACK
Because cardiogenic shock usually occurs in people who are having a severe heart attack, it’s important to know the signs and symptoms of a heart attack. These include:
- Pressure, fullness or a squeezing pain in the center of your chest that lasts for more than a few minutes
- Pain extending to your shoulder, one or both arms, back, or even to your teeth and jaw
- Increasing episodes of chest pain
- Shortness of breath
- Sweating
- Lightheadedness or sudden dizziness
- Nausea and vomiting
MULTIPLE ORGAN DYSFUNCTION SYNDROME

Multiple organ dysfunction syndrome (MODS) is a continuum, with incremental degrees of physiologic derangements in individual organs; it is a process rather than a single event. Alteration in organ function can vary widely from a mild degree of organ dysfunction to completely irreversible organ failure. The degree of organ dysfunction has a major clinical impact.
In a classic 1975 editorial by Baue, the concept of “multiple, progressive or sequential systems failure” was formulated as the basis of a new clinical syndrome. Several different terms were proposed thereafter (eg, multiple organ failure, multiple system organ failure, and multiple organ system failure) to describe this evolving clinical syndrome of otherwise unexplained progressive physiologic failure of several interdependent organ systems.
Eventually, the term MODS was proposed as a more appropriate description. MODS is defined as a clinical syndrome characterized by the development of progressive and potentially reversible physiologic dysfunction in 2 or more organs or organ systems that is induced by a variety of acute insults, including sepsis.
CENTRAL NERVOUS SYSTEM FAILURE

Central nervous system (CNS) failure represents a spectrum of disease ranging from mild neurological impairment that may have motor, sensory, visual, speech, cognitive manifestations, or a combination thereof, to comatose states and brain death.
COMMON CAUSES OF CENTRAL NERVOUS SYSTEM FAILURE
- Spontaneous Intracerebral Hemorrhage
- Metabolic / Infectious Derangements: liver failure, renal failure, Diabetic Ketoacidosis (DKA), meningitis.
A sudden (acute) nervous system problem can cause many different symptoms, depending on the area of the nervous system involved. Stroke and transient ischemic attack (TIA) are common examples of acute problems. You may experience the sudden onset of one or more symptoms, such as:
- Numbness, tingling, weakness, or inability to move a part or all of one side of the body (paralysis).
- Dimness, blurring, double vision, or loss of vision in one or both eyes.
- Loss of speech, trouble talking, or trouble understanding speech.
- Sudden, severe headache.
- Dizziness, unsteadiness, or the inability to stand or walk, especially if other symptoms are present.
- Confusion or a change in level of consciousness or behavior.
- Severe nausea or vomiting
The outcomes after being admitted in the ICU are very difficult to predict and most ICU doctors know patients among all the thousands who did RECOVER, against all the odds. The ICU team is there to save lives and by all means, prolong life. In reality, yes, odds are in a Patients favor according to the statistics, there are massive numbers of ICU patients who survived and let your loved one be part of the overwhelming majority of ICU patients who made it through. Allowing death in the ICU – even when there is still uncertainty about the outcome for the patient can be straightforward but you can be powerful advocates for keeping your loved one ALIVE even when doctors think otherwise! Take into account what the patient themselves would have wanted and that is, valuing the chance of life at any cost!
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips & strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care (it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Also, have a look at our membership site INTENSIVECARESUPPORT.ORG for families of critically ill Patients in Intensive Care here.
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!
REFERENCES:
- What Causes Organ Failure?
https://www.reference.com/science/causes-organ-failure-3c5d07f7260b3558
- Causes and Characteristics of Death in Intensive Care Units: A Prospective Multicenter Study
https://anesthesiology.pubs.asahq.org/article.aspx?articleid=2612636
- Multiple Organ Dysfunction Syndrome in Sepsis
https://emedicine.medscape.com/article/169640-overview#a3
- Organ failure: central nervous system
https://www.ncbi.nlm.nih.gov/pubmed/21989695
- Nervous System Problems
https://www.uofmhealth.org/health-library/nersp
- Cardiogenic shock
https://www.mayoclinic.org/diseases-conditions/cardiogenic-shock/symptoms-causes/syc-20366739
- Hospital Admitted Patient Care Activity, 2017-18
https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2017-18
- NATIONAL ADULT CRITICAL CARE CAPACITY AND ACTIVITY CENSUS 2016, HSE Acute Hospitals Division, Critical Care Programme.
https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/critical-care-capacity-and-workforce-census-2016.pdf
- Intensive Care Registries in Australia & New Zealand
https://healthmanagement.org/c/icu/issuearticle/intensive-care-registries-in-australia-new-zealand
- Variation in critical care services across North America and Western Europe*
https://pdfs.semanticscholar.org/d8d0/0f8fe3c58434b93518eb16d087e5413cde65.pdf
- Philip R. Lee Institute for Health Policy Studies, ICU Outcomes
https://healthpolicy.ucsf.edu/icu-outcomes
- The Location of Death and Dying Across Canada: A Study Illustrating the Socio-Political Context of Death and Dying
https://www.mdpi.com › pdf
- Case Mix Programme Summary Statistics 2015-2016
https://www.icnarc.org
- Intensive Care Registries in Australia & New Zealand
https://healthmanagement.org/c/icu/issuearticle/intensive-care-registries-in-australia-new-zealand
- Hospital Adult Critical Care Activity 2015-16, Table 10: Breakdown of critical care unit discharge status 1
https://digital.nhs.uk/data-and-information/publications/statistical/hospital-adult-critical-care-activity/2015-16







