What is heart failure?
Heart failure (HF), often called congestive heart failure (CHF) or congestive cardiac failure (CCF), occurs when the heart is unable to provide sufficient pump action to distribute blood flow to meet the needs of the body.Heart failure can cause a number of symptoms including shortness of breath, leg swelling, and exercise intolerance. The condition is diagnosed with echocardiography(Ultrasound of the heart) and blood tests. Treatment commonly consists of lifestyle measures such as smoking cessation, light exercise, dietary changes, and medications. Sometimes it is treated with implanted devices (Pacemaker or Ventricular Assist Devices) or ECMO(Extracorporeal Membrane Oxygenation) and occasionally a heart transplant.
Common causes of heart failure include Heart Attack(Acute Myocardial Infarction) and other forms of ischemic heart disease, hypertension, valvular heart disease, and Cardiomyopathy
The term heart failureis sometimes incorrectly used for other cardiac-related illnesses, such as Heart Attack(Acute Myocardial Infarction) or Cardiac Arrest which can cause heart failure but are not equivalent to heart failure.
Heart failure is a common, costly, disabling, and potentially deadly condition.In developed countries, around 2% of adults suffer from heart failure, but in those over the age of 65, this increases to 6–10%.
Heart Failure occurs when the heart is failing to move blood adequately around the body.
- What does the cardiovascular system do?
- Poor or abnormal function of the cardiovascular system
- Signs and Symptoms
- What happens in Intensive Care?
- Tests
- General Treatment Options
- How long will your loved one remain in Intensive Care?
- Internet Links


What does the cardiovascular system do?
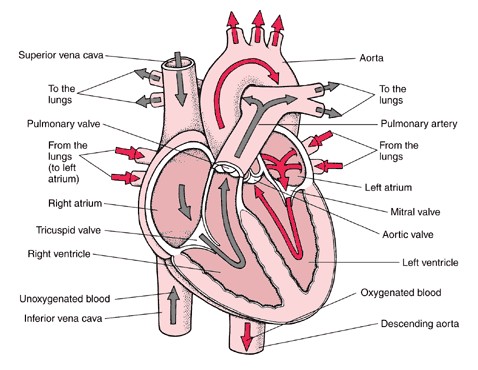
The essential components of the human cardiovascular system are the heart, lungs, blood, and blood vessels. It includes: the pulmonary circulation, a “loop” through the lungs where blood is oxygenated and the systemic circulation, a “loop” through the rest of the body to provide oxygenated blood. An average adult contains five to six quarts (roughly 4.7 to 5.7 liters) of blood, accounting for approximately 7% of their total body weight. Blood consists of plasma, red blood cells, white blood cells, and platelets. Also, the digestive system works with the circulatory system to provide the nutrients the system needs to keep the heart pumping.
The heart is at the centre, basically distributing blood from the ‘central pump’ with the blood vessels the pipes of the body, trying to reach every corner of the body. The cardiovascular system also passes nutrients (such as amino acids, electrolytes and lymph), gases(Oxygen and Carbon Dioxide), hormones, blood cells, etc. to and from cells in the body to help fight diseases, stabilize body temperature and pH, and to maintain blood pressure.
In the heart there is one atrium and one ventricle for each circulation, and with both a systemic and a pulmonary circulation there are four chambers in total: left atrium, left ventricle, right atrium and right ventricle. The right atrium is the upper chamber of the right side of the heart. The blood that is returned to the right atrium is de-oxygenated (poor in oxygen) and passed into the right ventricle to be pumped through the pulmonary artery to the lungs for re-oxygenation(inhalation) and removal of carbon dioxide(exhalation). The left atrium receives newly oxygenated blood from the lungs as well as the pulmonary vein which is passed into the strong left ventricle to be pumped through the aorta to the different organs of the body.The left side of the heart then receives oxygen rich blood from the lungs and pumps this blood into the Aorta and arteries of the body. This pumping action is a complex well-coordinated activity that cannot be fully explained here. The heart itself, receives oxygenated blood supply via the left and right coronary arteries.
This image was sourced using a google image search
Poor or abnormal function of the cardiovascular system
May be a result of:
May be a result of:
- Insufficient blood supply due to dehydration, bleeding or swelling;
- A poor blood supply to the heart, where there is not enough oxygen and other nutrients for its work;
- Poor lung function or obstruction to blood flow in the lungs, which places a strain on the heart muscle;
- Too many or too few electrolytes (eg. potassium, magnesium) that cause irregular heartbeats or dangerous rhythms in the heart.
- Weakness of blood vessel walls.
- Heart muscle weakness
- unhealthy lifestyle such as alcohol consumption, smoking, obesity
Signs and Symptoms
Signs
Left-sided failure
Common respiratory signs are tachypnea (increased rate of breathing) and increased work of breathing (non-specific signs of respiratory distress). Crackles, heard initially in the lung bases, and when severe, throughout the lung fields suggest the development of pulmonary edema (fluid in the alveoli). Cyanosis which suggests severe hypoxemia, is a late sign of extremely severe pulmonary edema.
Additional signs indicating left ventricular failure include a laterally displaced apex beat (which occurs if the heart is enlarged) and a gallop rhythm (additional heart sounds) may be heard as a marker of increased blood flow, or increased intra-cardiac pressure. Heart murmurs may indicate the presence of valvular heart disease, either as a cause (e.g. aortic stenosis) or as a result (e.g. mitral regurgitation) of the heart failure.
Right-sided failure
Physical examination may reveal pitting peripheral edema, ascites, and hepatomegaly(enlargement of the liver). Jugular venous pressure is frequently assessed as a marker of fluid status, which can be accentuated by eliciting hepatojugular reflux. If the right ventricular pressure is increased, a parasternal heave may be present, signifying the compensatory increase in contraction strength.
Biventricular failure(Left and Right Ventricular failure)
Dullness of the lung fields to finger percussion and reduced breath sounds at the bases of the lung may suggest the development of a Pleural Effusion(fluid collection in between the lung and the chest wall). Though it can occur in isolated left- or right-sided heart failure, it is more common in biventricular failure because pleural veins drain both into the systemic and pulmonary venous system. When unilateral, effusions are often right sided.
Symptoms
Heart failure symptoms are traditionally and somewhat arbitrarily divided into “left” and “right” sided, recognizing that the left and right ventricles of the heart supply different portions of the circulation. However, heart failure is not exclusively backward failure (in the part of the circulation which drains to the ventricle).
There are several other exceptions to a simple left-right division of heart failure symptoms. Left sided forward failure overlaps with right sided backward failure. Additionally, the most common cause of right-sided heart failure is left-sided heart failure. The result is that patients commonly present with both sets of signs and symptoms.
Left-sided failure
Backward failure of the left ventricle causes congestion of the pulmonary vasculature, and so the symptoms are predominantly respiratory in nature. Backward failure can be subdivided into failure of the left atrium, the left ventricle or both within the left circuit. The Patient will have dyspnea (shortness of breath) on exertion (dyspnée d’effort) and in severe cases, dyspnea at rest. Increasing breathlessness on lying flat occurs. It is often measured in the number of pillows required to lie comfortably, and in severe cases, the patient may resort to sleeping while sitting up. Another symptom of heart failure is paroxysmal nocturnal dyspnea a sudden nighttime attack of severe breathlessness, usually several hours after going to sleep. Easy fatigueability(tiredness) and exercise intolerance are also common complaints related to respiratory compromise.
“Cardiac asthma” or wheezing may occur.
Compromise of left ventricular forward function may result in symptoms of poor systemic circulation such as dizziness, confusion and cool extremities at rest.
Right-sided failure
Backward failure of the right ventricle leads to congestion of systemic capillaries. This generates excess fluid accumulation in the body. This causes swelling under the skin (termed peripheral edema or anasarca) and usually affects the dependent parts of the body first (causing foot and ankle swelling in people who are standing up, and sacral edema in people who are predominantly lying down). Nocturia (frequent nighttime urination) may occur when fluid from the legs is returned to the bloodstream while lying down at night. In progressively severe cases, ascites (fluid accumulation in the abdominal cavity causing swelling) and hepatomegaly (enlargement of the liver) may develop. Significant liver congestion may result in impaired liver function, and jaundice and even coagulopathy (problems of decreased blood clotting) may occur.
What happens in Intensive Care?
Patients with mild to moderate symptoms will generally be managed by the cardiac team in a coronary care unit (or combined ICU/CCU). However some Patients may present with severe symptoms and may require the full support of an ICU.
- Initially oxygen and respiratory support might be commenced via na oxygen mask or via Non- Invasive Ventilation(NIV) or BIPAP ventilation
- Full ventilation using a Ventilators(Breathing Machine) and a Breathing Tube (endotracheal tube) may be required to improve and maintain the oxygen delivery
- Sedation may be used if your loved one is in an induced coma
- Your loved one will require monitoring using a Bedside Monitors and an Arterial Catheter(Arterial Line)
- You can expect your loved one to have frequent Chest X-rays and blood tests(Blood& Pathology tests in Intensive Care) especially arterial blood gases (ABGs)
- Infusion pumps are administering drugs to support your loved ones blood pressure and haemodynamic system, as well as intravenous fluids may be administered via a central venous catheter/ CVC(Central Venous Lines)
- Use of a Pulmonary Artery Catheters or a PICCO catheter to closely monitor cardiac function is not uncommon.
- An NG Tube (Nasogastric Tubes) is usually inserted into your loved ones stomach, in order to commence nutrition or to remove fluids
- Urine Output is usually measured hourly, after insertion of a Urinary Catheter
- If your loved one has been admitted to Intensive Care with severe heart failure, LVAD/RVAD(Ventricular Assist Devices) or ECMO(Extracorporeal Membrane Oxygenation) therapy until the heart recovers may be commenced. Both, LVAD/RVAD or ECMO therapy may also be commenced for bridging to a heart transplant if considered appropriate
Tests that may be done in the Intensive Care Unit
- Physical Examination
- Chest X-ray
- Blood Tests(Blood& Pathology tests in Intensive Care)
- Urine tests
- ECG(Electrocardiograph)
- Echoecardiography(ultrasound of the heart)
Treatment options
Treatment of your loved one will depend on the severity of their presentation. Patients with mild to moderate symptoms will generally be managed by the cardiac team in a coronary care unit (or combined ICU/CCU). However some Patients may present with severe symptoms and may require the full support of an ICU. In a number of cases where the heart failure is extremely severe the doctors use mechanical devices to improve cardiac output (amount of blood the heart can pump) such as an Intra-Aortic Balloon Pump (IABP) or Ventricular Assist Devices. If your loved one deteriorates further ECMO(Extracorporeal Membrane Oxygenation ) may be a treatment option as well. Ventricular Assist Devices and ECMO Therapy are indicators that a heart transplantation may be necessary.
Drug Treatments
- ACE inhibitors (i.e., Enalapril, Captopril, Lisinopril, Ramipril)
- Beta Blockers(Metoprolol), to reduce Heart rate and reduce Blood pressure
- Diuretics(Frusemide, Aldactone) to increase Urine Output and treat fluid retention
- Vasodilators – dilate blood vessels which decrease the workload of the heart, I.e. GTN
- Antiarrhythmic drugs – keep the heart in a normal heart rhythm; I.e. Amiodarone, Digoxine
- Inotropic drugs -strengthen heart contraction, I.e. Noradrenaline, Adrenaline, Dobutamine, Milrinone
- Levosimendan to strengthen the contractility of the heart
How long will your loved one remain in Intensive Care?
The time your loved one needs to spend in Intensive Care/ Coronary Care depends on the severity of the heart failure and other pre-medical factors. Some Patients, especially if they require Intra-Aortic Balloon Pump (IABP), Ventricular Assist Devices or ECMO(Extracorporeal Membrane Oxygenation ) may require heart transplantation in the future.
Overall the length of stay of your loved one in Intensive Care or Coronary Care depends on whether the cause and the symptoms of the underlying heart disease can be treated effectively.
Internet Links
- http://www.heart.org/HEARTORG/
- Heart Health and Cardiac Rehabilitation (includes translation to Arabic, Greek, Italian, Russian and Spanish)
- National Heart Foundation – Australia
- NSW health Internet
- National Heart Foundation – New Zealand
- British Heart Foundation
- Heart Beat Victoria
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual Patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
Related Articles:
- How long does a cardiac arrest patient stay in Intensive Care
- Six weeks in Intensive Care after Cardiac Surgery and my mother isn’t getting any better…
- How long can a breathing tube or an endotracheal tube can stay in?
- How long should a Patient be on a ventilator before having a Tracheostomy?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Why does my loved one need a Tracheostomy in Intensive Care?
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- Be more selfish if your loved one is critically ill in Intensive Care
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- How long does it take to wake up from a Traumatic brain injury or severe head injury
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


