Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM, where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question last week was
You can check out the answer to last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer another frequently asked question from our readers and the question this week is
How to wean off ECMO?
So let’s look at this question in more detail.
Today’s episode of “YOUR QUESTIONS ANSWERED” is a little bit more technical in nature compared to other episodes.
But more and more families in Intensive Care want to know about ECMO and they have specific questions and I want to answer specific questions with specific answers!
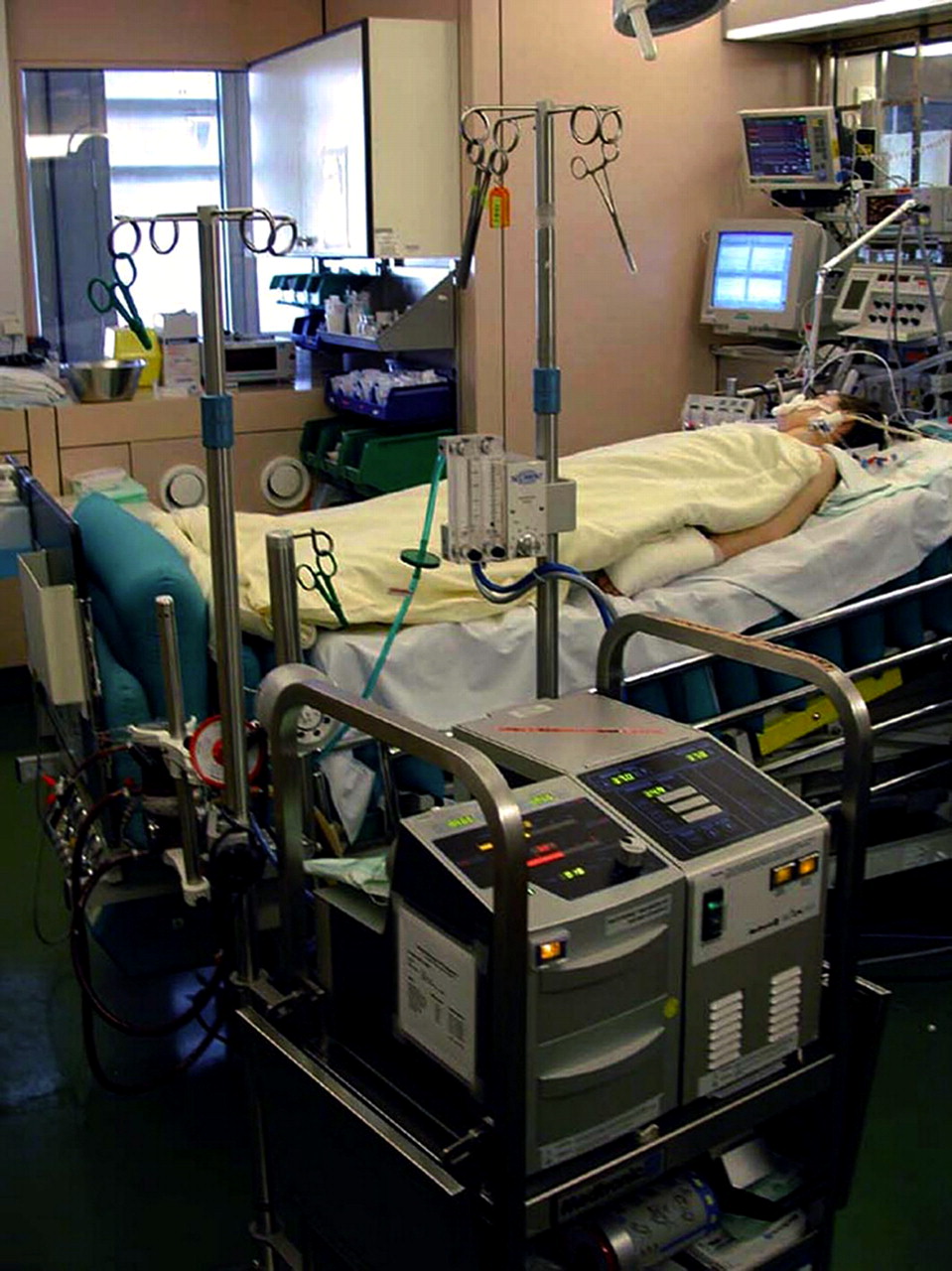
More and more critically ill Patients require ECMO for either heart failure or lung failure(ARDS).
If you haven’t heard about ECMO and you don’t know what it is please check out our section about ECMO here.
https://intensivecarehotline.com/ecmoextracorporeal-membrane-oxygenation/
I have also written a blog about “How long can a critically ill Patient stay on ECMO?”
Let’s just quickly look at ECMO in general. ECMO stands for Extra-Corporal-Membrane-Oxygenation and it replaces the function of the heart or the lungs in critically ill Patients.
You may have heard me explain before that all major organs(except the brain) of the body in a critically ill Patient in Intensive Care can be controlled at least temporarily.
ECMO can do that in heart failure and in lung failure/ARDS, it can control and take over the function of the heart or the function of the lung for a period of time.
ECMO for heart failure is also classified as VA-ECMO and ECMO for lung failure/ARDS is classified as VV-ECMO.
Again for more general information about ECMO and the exact differences between VA-ECMO and VV-ECMO please check out our general ECMO section here
https://intensivecarehotline.com/ecmoextracorporeal-membrane-oxygenation/
and check out this article/video here
HOW LONG can a critically ill Patient stay on ECMO?
What’s important for you and your family to know that if ECMO for either heart failure or lung failure can’t be weaned there are two to three other options as well that you need to know about. Sometimes Intensive Care teams may or may not be transparent about these options and therefore I want to bring them to you in this blog.
- In VV-ECMO for lung failure/ARDS, if ECMO can’t be weaned because of the lungs not recovering, ECMO can be a bridging therapy towards a lung transplant. I.e. I have seen some critically ill Patients going on ECMO for lung failure/ARDS for a few days, up to two weeks and in one case for less than 24 hours before a lung transplant became available. There is a risk that if VV-ECMO is commenced for lung failure/ARDS and a lung transplant is not becoming available that ECMO might be futile(=to no benefit of the Patient) and a critically ill Patient might pass away
Find more information about lung transplants here
- In VA-ECMO for heart failure, if ECMO can’t be weaned because of the heart not recovering and remaining de-compensated, ECMO can be a bridging therapy to a VAD(=Ventricular assist device) and/or heart transplant. Patients requiring a heart transplant tend to require more preparation and time, also because of donor hearts not being as readily available as donor lungs, therefore a VAD is a good device to buy time and prepare Patients for a heart transplant. Many Patients can even go home on a VAD and await a heart transplant at home
More info about VAD and heart transplant here(click on the links)
Now let’s look at weaning ECMO
- Weaning VV-ECMO for lung failure/ARDS
Patients requiring VV-ECMO for lung failure/ARDS are usually mechanically ventilated with a breathing tube(endotracheal tube) or tracheostomy. However whilst being on VV-ECMO the support from the ventilator(breathing machine) tends to be reduced to a bare minimum because of the ECMO machine regulating the gas exchange that normally takes place in the lungs. Therefore by gradually reducing the pump flow of the ECMO machine and by gradually reducing the oxygen supply of the ECMO machine, the support on the ventilator will be gradually increased and assessed for its effectiveness.
During VV-ECMO for lung failure/ARDS the support from the ventilator(breathing machine) tends to be reduced so that the lungs can rest and heal.
If a reduction of the flow from the ECMO machine can be adequately replaced by the ventilator and all vital signs and parameters stay within normal limits, ECMO is ready to be discontinued.
This will be done by assessing the ventilation parameters as well as ABG’s(=Arterial blood gas to assess the oxygen and CO2/Carbon-dioxide in the blood) and chest X-rays.
Once the ventilator can provide adequate gas exchange(=oxygen/O2 vs Carbon-dioxide CO2) for a critically ill Patient in lung failure/ARDS, ECMO can be removed.
In essence, once the lungs can adequately start functioning again with the support from the ventilator, ECMO can be removed.
It is very important and critical to make thorough assessments before removing VV-ECMO for lung failure/ARDS because it’s high risk putting ECMO back in if removal of ECMO fails.
- Weaning VA-ECMO for heart failure
When weaning VA- ECMO for heart failure, formal weaning studies need to be performed before removing VA-ECMO.
The simple reason for formal weaning studies is that intrinsic or native heart function must be assessed first.
Again, just like in VV-ECMO for lung failure, ECMO is taking over the function of the heart.
In severe heart failure, critically ill Patients have minimal to no cardiac output and their ejection fraction(= is a test that determines how well your heart pumps with each beat) is minimal.
Therefore native or intrinsic heart function is minimal and without ECMO the Patient with heart failure is at high risk of dying.
Normally in heart failure and VA- ECMO, inotropic medications such as Dobutamine, Milrinone, Levosimendan, Noradrenaline and/or Adrenaline are given to support contractility of the heart and also to increase blood pressure.
In VA- ECMO for heart failure, the procedure to wean off VA- ECMO needs to follow a few steps
- Perform Echocardiogram(=Ultrasound of the heart)
- Perform TOE(=transesophageal echocardiogram, or TEE (TOE in the United Kingdom, reflecting the spelling transoesophageal), is an alternative way to perform an echocardiogram. A specialized probe containing an ultrasound transducer at its tip is passed into the patient’s esophagus to perform an ultrasound of the heart closer to the source)
- Wean the pump flow of the ECMO machine and find out if native/intrinsic heart function is improving and maintaining a physiological and life sustaining cardiac output(=measurement of the amount of blood that is pumped out of the heart in one minute)
- Check ABG’s(=arterial blood gases to assess adequate oxygen and CO2/Carbon-dioxide levels in the blood)
- Assessment of ejection fraction with Echocardiogram and/or TOE
- Lung ventilation must be increased, this is similar to VV-ECMO
If weaning off VA-ECMO for heart failure fails, again a bridging therapy to a VAD is often possible. A VAD might buy time and prepare for a heart transplant. Just like in VV-ECMO for lung failure/ARDS, premature removal of ECMO therapy for heart failure is highly risky and can be lethal, because it’s high risk putting ECMO back in if removal of ECMO fails.
Also, it is very very rare that during either VA-ACMO or VV-ECMO a critically ill Patient is not being ventilated and in an induced coma.
I hope this clarifies and now you know how ECMO is being weaned. Any other questions please send to [email protected]
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips& strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care(it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!



