Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM , where we instantly improve the lives of Families of critically ill Patients in Intensive Care, so that you can have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question last week was PART 5 of
“MY AUNTY IS IN INTENSIVE CARE ON ECMO FOR ARDS, WE’RE VERY WORRIED SHE MAY DIE! HELP!” (PART 5)
You can check out the answer to last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer another question from one of our readers and the question this week is PART 6 of
“MY AUNTY IS IN INTENSIVE CARE ON ECMO FOR ARDS, WE’RE VERY WORRIED SHE MAY DIE! HELP!” (PART 6)
Lee from the UK writes
Hi Patrick,
we’ve been back to the hospital today and my auntie was quite bad overnight with gases in the blood.
Today however they have managed to remove all gases and its at 100 % normal levels and they are draining 150ml of fluid per hour off her by dialysis to help drain the fluid.
She isn’t passing any urine herself but I think that’s because of oxygen requirement levels.
Her ventilation support was as low as 30 % oxygen today but was back to 50% by the time we had left. We were told this was normal after physio and will probably be reduced later.
Her lungs are still wet and they said they will keep draining her by dialysis in the hope that the dryer she gets the less support she will need and that will allow her lungs to expand more and hopefully repair itself.
They think there is an underlying problem from her original diagnosis Pneumonia, but normally patients would have been off ECMO and got rid of the Pneumonia by now and they can’t understand why this is.
They said that they will keep drying her until they can identify the cause and if they can treat it they will if it’s treatable.
We spoke with the ECMO team and she has not got any chance to go on ECMO back at all, because she wouldn’t last on that and also because she has been asleep for so long and on the ventilator for such a long time and that they apparently know through past experiences. They said also you can’t go on ECMO after you have been off it for so long.
Today we spoke to her consultant who was very keen with questions about my aunties mental health and has she ever had quite a long period without her tablets.
Although she has been diagnosed with schizophrenia and she is on medication for this.
Quite a few of her support workers over the years and also my mum questions whether she actually is schizophrenic, as she only ever has thoughts now and then and not actually verbally hears or sees people.
Also during support groups she attends, she doesn’t display the same behaviour as them or has the same manerisms or just doesn’t seem the same at all just like she suffers from a bit of depression and enjoys the company.
She is currently on sodium valproate and diazepam when required does this give her a low cell count and immune system? Is it relevant in any way?
Would stopping one or more of these medications make any difference?
She has an infection as well but not sure what infection and infection markers are coming down slowly.
They also asked if they can’t find a solution what we think about a lung transplant?
They said that it’s a long process and there is a very long waiting list and that’s not to say they would even accept her on to the lung transplant waiting list.
Thanks
Lee
Hi Lee,
thanks for the update.
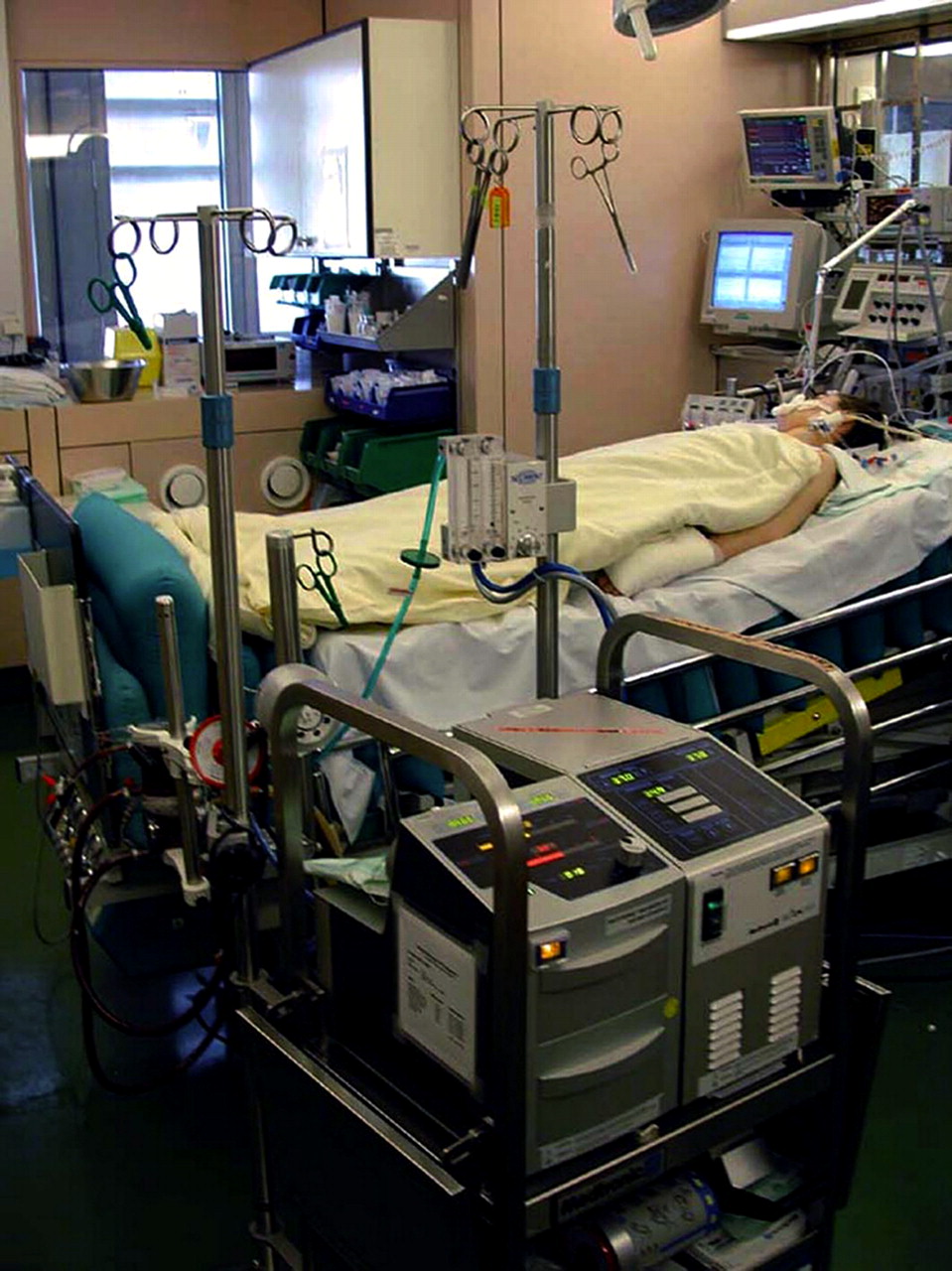
The most important thing that stands out to me in your email is that the ECMO team says, that your aunty can’t go back on ECMO.
That is complete and utter BS. I have seen many Patients who have gone back on ECMO after they have been on it before.
I believe the Intensive Care team/ ECMO team is trying to plant a seed there for you and your family that she can’t have it back for whatever reason.
There is absolutely no reason why your aunt can’t go back on the ECMO. The only reason why she couldn’t go back on it would be the low Platelets or any other issue with her blood being too thin and that could cause severe bleeding on ECMO. That would be the only risk that would make it almost impossible for your aunty to go back on ECMO.
Unless there are other reasons that you haven’t mentioned that would stand in the way of going back on ECMO.
Also, it is complete and utter nonsense to say that your aunty can’t go back on ECMO because “she has been asleep for so long and on the ventilator for a long time and through past experiences. they said also you can’t go on ecmo after you have been off it for so long. “
Again, this is BS and I have seen Patients being on ECMO for up to 3 weeks and that time period would have included Patients coming on and off ECMO within those 3 weeks.
Again check out this article here
It is certainly a relatively high risk to back on ECMO if needed and one has to certainly weigh up pros and cons before making such a decision, but the reasons they are giving you are nonsense.
Ask them about their past experiences, let them give you the facts.
There is absolutely no reason why your aunt can’t go back on ECMO, even after “she’s been off it for so long”.
Also, the mental illness of your aunty should not be a point of discussion on what type of treatment she gets while she is in Intensive Care. I wouldn’t even go there if I was you, unless you feel that it’s relevant.
If the Intensive Care team thinks that the mental illness of your aunty is relevant for what type of treatment she is getting or not getting, whilst being critically ill in Intensive Care, you need to ask a few simple and very effective questions in order to determine your next courses of action
- Has your aunty or anybody in your family ever mentioned that she doesn’t want to live?
- Has your aunty documented an advanced care plan, i.e. does she want to have certain things done or not done in case such a crisis like she is in now emerges?
The answers to these questions should be determining in how you position your aunt and how you advocate for her!
Don’t worry in how the Intensive Care team or the ECMO team positions your auntie’s prognosis and diagnosis, because it sounds to me like they are looking at her mental illness, as well as her ICU stay to be the determining factor in what they offer or don’t offer in her current situation.
I would almost argue that by “only” having your aunt on ECMO for 6 days initially wasn’t enough in order to let her lungs heal and rest after the ARDS. Most Patients that I’ve seen on ECMO for ARDS had been on it for at least one week or more in order to give enough time for the lungs to heal.
It gives, in essence the lungs more time to heal and rest.
Also, they can’t tell you that ECMO might be unavailable. Whenever there is a crisis, especially in peak winter times with flu, Pneumonia etc… where ECMO could be a “live safer”, usually ECMO machines can be made available from the manufacturers themselves in order to facilitate demand.
Going back to what happened yesterday, overall it doesn’t sound like you need to panic though.
Oxygen demands can go up and down and if her oxygen requirements stay between 30% to 50% that’s actually not too bad and on those oxygen levels there is no need for ECMO anyway.
Again, given that your auntie’s lungs are still wet, it’s also a sign that the ARDS is persistent. If you have read through our section about ARDS here https://intensivecarehotline.com/clinical-pictures/adult-respiratory-distress-syndrome-ards/ you can see why the lungs would still be wet.
It’s good that they keep using the Dialysis machine and drain fluids.
Also, as far as the lung transplant goes, lung transplant is a last resort, after ECMO has failed. But you need to be prepared and you need to be able to argue your auntie’s case in case things don’t go well.
Again, things happen slowly in ICU. It sounds like your aunt isn’t going backwards. 30- 50% Oxygen requirements isn’t too bad and keeps her away from ECMO for now. Be patient. Again, read through Ellie’s questions, it could well be that you are just at the beginning of a journey.
You can read Ellie’s questions here:
As far as the medications for your auntie’s mental illness go, I couldn’t tell you how they affect her current situation, however it is unlikely that those medications interfere with what’s currently happening clinically.
Again, as I mentioned before, your aunt’s mental illness should be out of the equation for now, as she is battling much bigger issues. Keep this in mind, as long as she is fighting for her life.
Her mental health issues should not be becoming an issue as long as she is critically ill.
We are talking about death or life here and not about a mental illness.
If you and your family think that she wouldn’t want to live because of her mental illness then you might have to rethink your strategies and as long as that’s not the case, you need to reframe and re- emphasize your positioning to the Intensive Care team and ask for nothing but the best!
Also, here are a few articles about induced coma and how long critically ill Patients can stay in an induced coma so that you are well informed
Here is a link to another article that might help you to stay focused and get what you want
So stay strong, always keep making up your own mind and don’t give up!
Thank you& Kind Regards
Patrik
How can you have PEACE OF MIND, control, power and influence whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care! Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below!
In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips& strategies helping you to get on the right path to PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care(it’s not what you think)
Thank you for tuning into this week’s “YOUR QUESTIONS ANSWERED” and I’ll see you again in another update next week! Make sure you also check out our BLOG section for more tips and strategies or send me an email to [email protected] with your questions!
You can also call us, check out our international phone numbers here.
Also check out our Products section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 consulting with me!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!
Related Articles: