Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS
Hi, it’s Patrik Hutzel from INTENSIVECAREHOTLINE.COM, where we instantly improve the lives for Families of critically ill Patients in Intensive Care, so that you can make informed decisions, have PEACE OF MIND, real power, real control and so that you can influence decision making fast, even if you’re not a doctor or a nurse in Intensive Care!
This is another episode of “YOUR QUESTIONS ANSWERED” and in last week’s episode I answered another question from our readers and the question last week was
My Mother in law is in ICU with seizures and a brain tumour! She’s not waking up, can she survive?
You can check out the answer to last week’s question by clicking on the link here.
In this week’s episode of “YOUR QUESTIONS ANSWERED” I want to answer another question from one of our readers and the question this week is
My 40 year old brother has been in ICU for 4 weeks after bowel obstruction and Sepsis! He’s still ventilated with tracheostomy and I don’t want him to die, help!
This question from Kerry formed part of an email counselling/consulting session with me.
Kerry writes
Hi Patrik,
a month ago we took my 40 year old brother to the emergency room where they discovered he had a bowel obstruction! He was flown to a larger medical centre who is more equipped to do the surgery which was behind his pancreas.
My brother has a long standing pre-medical history such as Oesophagus cancer in 2012 – treatment included chemotherapy, radiation, surgical intervention over the course of a year and a half. From 2013 to present he’s had clear CT scans and no signs of cancer.
He also has been Bi-Polar for many years which has been left untreated.
Alcoholism untreated from teen years until present (40 years old) Drug abuse Smoking – from teen years until present.
When we took him to the Hospital he had issues breathing and the surgery took 8 hours. He was approaching cardiac arrest within the first night but they intervened in time and stabilized him.
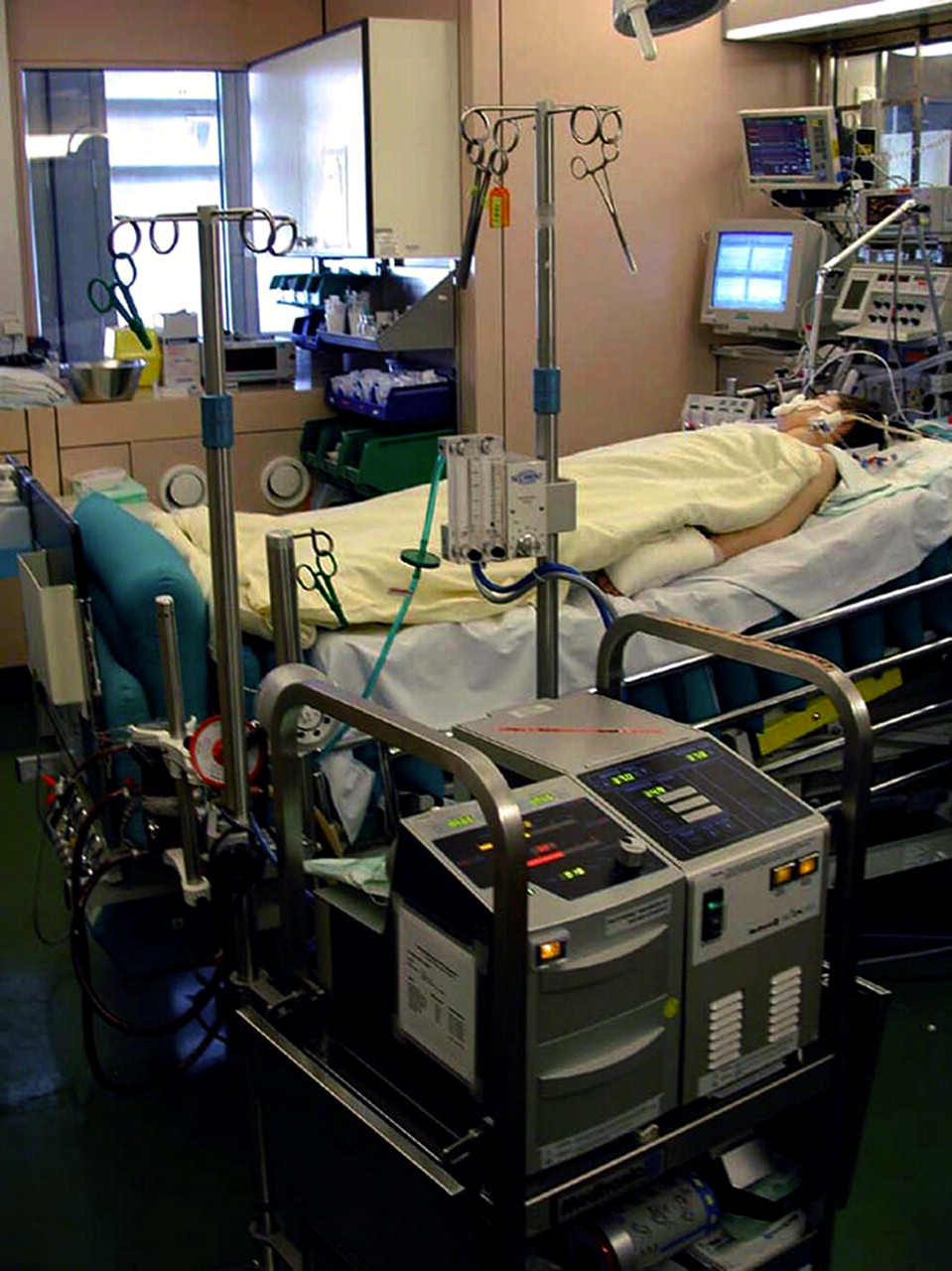
He has been in ICU since the surgery and has since the surgery not been able to breathe without a ventilator therefore he has a tracheostomy in place.
They tried for a day or two but did not have any success weaning him off the ventilator. Also, he has a pleural effusion – unsure of the source or cause – a tube is in place draining the fluid.
He had a PICC line in for antibiotics to flow directly closer to his heart? As well it was discovered after the surgery he had a severe pneumonia. His kidney function is low and not stable – they have been monitoring it.
He’s had two CT scans and the liquid discharge from the lungs has been sent for further testing.
We received a call from the Social Worker in ICU asking historical questions as he cannot speak with the tracheostomy, he can only nod ‘yes’ or ‘no’.
He wrote one note that said “I will be dead soon”. He’s attempted to rip the tubes out therefore prompting sedation and restraint. The message we got from the Social Worker was that he’s been through a lot in the past few years, his muscles are wasting being in bed and they cannot do any physiotherapy as he does not have the strength to be out of bed nor breathe on his own.
The social worker told us that the more time he spent in the ICU the less likely recovery will be to the point of functioning prior to admittance. As for his note about dying she said sometimes people have premonitions and that he may or may not die.
I’m not sure how to take all of this, I’m 8 hours away from this Hospital and rely solely on phone conversations with nurses and occasionally I get to speak to a doctor, if I’m lucky.
I have major concerns and am worried I will get a phone call things have turned for the worse, make decisions for him and get there if I can or along those lines.
My mother died in 2013 after having open heart surgery and not recovering, she had breast cancer that spread to the pleural fluid in her lung wherein she required the same tube for drainage. She also was in Intensive Care for a month and a half, her kidney function was low as well, as her blood pressure dropped continuously.
One night I got a phone call that she was not doing well, I went into the ICU and I was told she was experiencing multi organ failure, her body was shutting down and she passed away that night.
I know this is a different circumstance but I am worried and again experiencing the same issue – no answers, no direction, no idea if there is a chance of recovery or exactly how severe this is.
Do you have advice on how to talk to the ICU doctors and nurses? If there are any things I should be asking that I’m missing etc?
I’m at a loss and feel like I’m back in the same loop I was with my Mom which ultimately lead to her death.
Thanks for your time!
Kerry
Hi Kerry,
thank you for using my 1:1 email counselling and consulting services!
I’m very sorry to hear about this difficult situation that your brother and also yourself are currently dealing with!
The circumstances are certainly very difficult especially since you are 8 hours away from the hospital where your brother is currently at.
Let’s look at your and your brother’s situation in detail and I will break this down for you step by step so that you have more information at hand and also have some action steps so that you know what you need doing!
First, your brother had the bowel obstruction and he had to have emergency surgery for that. You mentioned that he approached cardiac arrest and that they stabilized him just at the right time to prevent him from going into cardiac arrest.
He most likely approached cardiac arrest because he had a severe infection or Sepsis due to the bowel obstruction and his blood pressure would have dropped significantly and therefore he would have been at high risk to go into cardiac arrest!
The good news for now is that your brother is alive and whenever there is life there is hope!
Your brother’s overall situation is certainly challenging, especially with his long-standing and significant pre-medical history at such a young age!
I can also see that your negative experience with your mother’s death in ICU is weighing heavily on your current thought processes and it’s probably also why you are seeking out professional help through me!
It must have been a traumatic and nightmarish experience for you having seen your mother in Intensive Care for a month and a half suffering and then pass away! Given that this has been a relatively recent experience, it’s still fresh in your mind and you don’t want to repeat this experience!
Given that I have lost close family members myself in the past within short periods of time, I have first-hand experience in how you must feel given that you are facing an almost similar situation with your brother!
Your brother is certainly in a difficult, challenging and certainly life threatening situation from what you are describing!
What speaks for him is his young age and what’s also speaking for him is that he survived Oesophagus cancer! That’s telling me that he’s a fighter and that he can deal with adversity!
He certainly has other medical challenges and issues and I will come to that in a moment and explain to you how it might impact on his current situation!
You are mentioning that your brother has a PICC line (=central line) and the reason for that is that he will need ongoing Antibiotic therapy until his infection has been cleared. Furthermore there is a very high chance that your brother is or has been on Inotropes for his low blood pressure, therefore he most likely will need the PICC line for some time to come. The good news is that a PICC line can stay in for up to three months and therefore they have done the right thing to insert the PICC line!
And yes a PICC line, just like a central line, have the intravenous drugs go directly to the heart to be more effective!
Furthermore, you have also mentioned that your brother has a tracheostomy in place and that he’s still on the ventilator as they have had not much success to wean him off the ventilator thus far.
Weaning your brother off the ventilator and the tracheostomy might take time. Given that he has a significant and long-standing pre-medical history this might work against him getting off the ventilator quickly.
Especially his long-standing drug and alcohol abuse may stand in his way of achieving weaning off the ventilator quickly as he might lack the strength to get weaned quickly.
I have seen this over and over again that critically ill Patients in Intensive Care get weaned very slowly if they have a history of drug and alcohol abuse. Their overall condition tends to be weakened and therefore things are lot slower and more challenging.
Moreover you also mentioned that your brother now has a Pneumonia as well as a Pleural effusion.
Developing a Pneumonia after being ventilator dependent for such a long time as well as having a long-standing pre-medical history make it all the more likely to develop a Pneumonia. Again it’s most likely another one of the reasons he’s having a PICC line in order to get Intravenous Antibiotics for treating the Pneumonia!
It’s also very likely that the Pleural effusion your brother is dealing with is a result of having a low Albumin in his blood as well as having a Pneumonia.
Usually what happens is that critically ill Patients with a history of drug and alcohol abuse also experience a degree of liver failure and therefore they often develop a Pleural effusion due to low Albumin in the blood which is a result of the liver failure.
To a degree it doesn’t surprise me that your brother is trying to rip off the chest tubes because he is most likely confused since he’s been in ICU for so long. Most critically ill Patients in Intensive Care who have been in an induced coma go through significant periods of confusion and I will talk more about that in a moment.
The chest drains are draining the Pleural effusion and it’s therefore taking the pressure off the lungs, helping his Pneumonia as well.
Both, the Pleural effusions and the chest tubes as well as the Pneumonia are not increasing the chances that he will get off the ventilator anytime soon.
Related article/video
TRACHEOSTOMY AND WEANING OFF THE VENTILATOR IN INTENSIVE CARE, HOW LONG CAN IT TAKE?
Therefore the Pleural effusion will need to be drained first and his Pneumonia will need to be cured as well before he’s ready to move forward.
You have also mentioned that your brother is in kidney failure or at least at the early stages of kidney failure. This is again nothing surprising to me, given that by now he’s been in ICU for more than one month.
The longer Patients stay in Intensive Care the higher the chance for kidney failure. Kidney failure can occur for a number of reasons including but not limited to
- Low blood pressure and Sepsis
- Medications given resulting in undesirable side effects such as kidney failure
You are saying that they are currently monitoring it, therefore this is an indication that they don’t need to intervene as yet, besides most likely already giving Diuretics such as Frusemide(Lasix) to increase Urine output to keep the kidneys going.
As long as they don’t need to use the Dialysis machine to treat the kidney failure, there is a good chance that your brother’s kidney failure is low grade kidney failure.
One of the big challenges that any critically ill Patient in Intensive Care is dealing with when they are ventilated and have a tracheostomy is their inability to communicate properly.
This why they are often depressed and lethargic.
It certainly doesn’t help that your brother is needing intermittent sedation and restraints. If that happens it usually sets Patients back in their attempts to be weaned off the ventilator and the tracheostomy.
Keep in mind that one of the reasons a tracheostomy is inserted in the first place is to minimise sedation!
Furthermore, you have already pointed out that your brother is getting weaker and weaker whilst he is staying in bed and on the ventilator!
It’s very sad to hear that they haven’t started Physiotherapy and I’m very disappointed to hear that. From my perspective there is absolutely no reason why they can’t start Physiotherapy. They can surely start mobilising your brother in a chair by sliding him into a recliner chair. They can also start moving his arms and legs even when he’s in bed.
I’m very frustrated to hear that because most ICU’s that I have worked in, early Physiotherapy has always been important and also effective!
Another issue that your brother is facing is that he may have real fear of death which is why he may have written a note about him dying soon. However, there is also a very good chance that your brother is not only withdrawing from alcohol or drugs, he may well also withdraw from the sedatives and opiates he would have had whilst he was in an induced coma.
On top of that he’s dealing with an untreated Bi-polar disorder making it all the more likely that he would be disoriented and confused.
It would be very difficult for any Intensive Care team to treat a Bipolar disorder that has been untreated in the past. Therefore all the Intensive Care team can do for now is to make sure he stabilises and gets out of his delirium. This can be achieved with medications, however it will be all the more challenging if they keep restraining him and give him more sedation.
Related article/ video:
The way forward is to start mobilising your brother, make sure he gets into a day and night rhythm, meaning he’s awake during the day and goes to sleep at night. A good and undisturbed day and night rhythm will help your brother to get stronger and also to get weaned off the ventilator.
There is also a very good chance that your brother is currently going through a delirious phase or also classified as ICU Psychosis, which again is nothing unusual after having spent so much time in Intensive Care, in an induced coma and on a ventilator.
Just from what you are describing with restraints and more sedation make it all the more likely that your brother is exactly going through that and it’s often difficult and challenging to get critically ill Patients through that phase.
He will need a lot of attention, understanding and “tender loving care” to help him through that situation, especially since your brother may still be withdrawing from alcohol, drugs and also some of the sedatives and opiate drugs! Therefore you may have to be a bit more patient.
Only when he has overcome the delirium and confusion is he really ready to move on and to be weaned off the ventilator.
Recommended:
Again, I can’t stress enough how important it is to start mobilizing your brother and start the Physiotherapy. Other things such as good nursing care, regular washes and regular showers are extremely important as well! General well being is very important and can be achieved relatively easily by people making an effort!
Good nursing care as well as Physiotherapy are much better than any sedatives or any other medication and can work wonders!
As a rule of thumb, you’ve got to be prepared to take two steps forward and one step back, especially since your brother’s situation is very challenging!
As far as your communications with the doctors and the nurses go, you’ve got to be prepared to make them accountable for their actions as well as results and outcomes or lack of such.
It’s very difficult in your situation because you are 8 hours away and currently you can only communicate via phone.
It’s probably best if you start by writing down some names from the key people who are involved in the care of your brother and try and start talking to them regularly. I would suggest you refer to the treating consultant and/or to the nurse in charge. A social worker might be a good contact as well, however they generally don’t know enough about the clinical issues.
Recommended:
You now have enough information to ask the right questions and challenge the Intensive Care team on every level.
You should also ask for a telephone conference with a couple of the key people, I.e. treating consultant, nurse in charge and the social worker. This is essential, especially since you are in a different location. You will want to get a feeling who the people are that you are dealing with!
I would of course also recommend that you’d go and visit your brother, however I obviously don’t know if this is an option for you?
It really boils down to you keeping the communication channels open with your brother’s care givers and trying to get things moving in the right directions!
I can really empathize how you feel, especially since you’ve had this traumatic experience with your mother passing away in ICU in 2013.
And I can see how this experience weighs heavily on your current view of your brother’s situation. You don’t want to experience another phone call in the middle of the night with devastating news!
However, what I always say is this! Stay positive! Staying positive is half of the battle and it often makes all the difference.
Related article/video:
This time you are getting informed and this time you are seeking professional help, therefore you are in a much better position compared to when your mother passed away!
You now have a much better understanding of what you can control, therefore make use of that knowledge to your advantage!
Last but not least, if your brother can’t be weaned off the ventilator and the tracheostomy, you should start thinking about alternatives! Home care might be one option. INTENSIVE CARE AT HOME is offering a genuine alternative to a long-term stay in Intensive Care for long-term ventilated adults& children in Intensive Care!
INTENSIVE CARE AT HOME can provide at home what Intensive Care Units can do. This provides a win-win situation and offers a lot more quality of life for long-term ventilated adults& children with tracheostomies and their families.
It makes a lot of sense, home care instead of Intensive Care.
Check out INTENSIVE CARE AT HOME for more information.
I hope that helps Kerry, please let me know if you have any other questions!
Wishing you and your family all the very best!
Your friend
Patrik
How can you become the best advocate for your critically ill loved one, make informed decisions, get peace of mind, control, power and influence quickly, whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of making informed decisions, get PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below!
In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to make informed decisions, get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care!
Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below! In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care! In your FREE report you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 mind blowing tips& strategies helping you to get on the right path to making informed decisions, get PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘behind the scenes’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care(it’s not what you think)
Thank you for tuning into this week’s YOUR QUESTIONS ANSWERED episode and I’ll see you again in another update next week!
Make sure you also check out our “blog” section for more tips and strategies or send me an email to [email protected] with your questions!
Or you can call us! Find phone numbers on our contact tab.
Also check out our Ebook section where you get more Ebooks, Videos and Audio recordings and where you can also get 1:1 counselling/consulting with me via Skype, over the phone or via email by clicking on the products tab!
This is Patrik Hutzel from INTENSIVECAREHOTLINE.COM and I’ll see you again next week with another update!
Your Friend
Patrik Hutzel