- What is a Bronchoscopy?
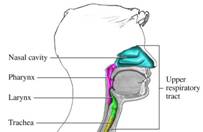
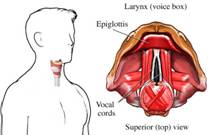
Bronchoscopy is a procedure where the inside of the lungs or airways are visualised for diagnostic and therapeutic purposes. A bronchoscope(sterile instrument with with video camera) is inserted into the lungs or airways, usually through the nose or mouth, or occasionally through a Tracheostomy. This allows the practitioner to examine the Patient’s lungs or airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Sputum specimens for infection testing may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with real time video equipment.
- Why is a Bronchoscopy done?
- What happens in Intensive Care?
A bronchoscope. Image found at Google images

Why is a Bronchoscopy done?
Bronchoscopy allows for assessment and evaluation of the upper airway structures. A Bronchoscopy can be either diagnostic or therapeutic;
If a Bronchoscopy is done fo diagnostic purposes it is
- To view abnormalities of the airway
- To obtain tissue specimens of the lung in a variety of disorders. Specimens may be taken from inside the lungs by biopsy, bronchoalveolar lavage, or endobronchial brushing.
- To evaluate a person who has bleeding in the lungs, possible lung cancer, a chronic cough or sarcoidosis
If a Bronchoscopy is done for therapeutic purposes it is
- To remove secretions, blood, or foreign objects lodged in the lungs or airway
- Laser resection of tumors or benign tracheal and bronchial stenosis
- Stent insertion to palliate extrinsic compression of the tracheobronchial lumen from either malignant or benign disease processes
- Bronchoscopy is also employed in percutaneous Tracheostomy
- Tracheal Intubation of Patients with difficult airways is often performed using a flexible bronchoscope

Images found at WebMD
What happens in Intensive Care?
The bronchoscopy should be explained to your loved one and the family with rationales for the procedure. It also requires your loved ones or your consent. In Intensive Care your loved one will be given sedation(Propofol, Midazolam) and pain relief(Fentanyl) during the procedure so he or she will be asleep and not feel any pain. In Intensive Care a Bronchoscopy most of the time is done on Patients who are already mechanically ventilated on a ventilator(Ventilators/Breathing Machines) and who either already have a Breathing Tube or Endotracheal Tube or a Tracheostomy in place. Through either the Breathing tube or the Tracheostomy, access to the lungs is relatively easy. The bronchoscopy is passed into the tube, and then into the airway/lungs.
During the procedure your loved one is constantly observed and their vital signs are constantly monitored and displayed using Bedside Monitors. Once the bronchoscope with the video camera is inserted into the lungs/airways each part of your loved ones airway is looked at and screened for any abnormalities. If anything abnormal is discovered, they may take a tissue sample using a brush, needle or forceps. This will be sent to the laboratory for diagnosis.
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
References
Belli MA. Critical care extra. Bronchoscopy. American Journal of Nursing. 1999 Jul; 99(7)
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual patient. Please refer to the full disclaimer.
Related articles:
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- How long can a breathing tube or an endotracheal tube can stay in?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Why does my loved one need a Tracheostomy in Intensive Care?
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- Be more selfish if your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 4 ways on how to be more persuasive if your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- How long does it take to wake up from a Traumatic brain injury or severe head injury
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


