Respiratory Conditions- Pleural Effusion
What is a Pleural Effusion?
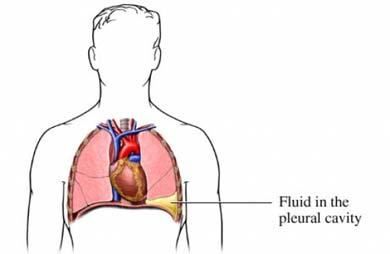
Pleural effusion is excess fluid that accumulates between the two pleural layers, the fluid-filled space that surrounds the lungs. Excessive amounts of such fluid can impair breathing by limiting the expansion of the lungs during ventilation. The types of fluids that accumulate in the lungs are caused by
- Haemothorax – a collection of blood usually as the result of chest trauma
- Chylothorax – a collection of lymphatic fluid
- Para pneumonic effusion – a collection of exudate associated with an infective process such as Pneumonia
- Empyema – a parapneumonic effusion with pus
- What does the Respiratory system do?
- Abnormal and or inadequate breathing
- Diagnosis
- Signs& Symptoms
- Treatment
- What Happens in Intensive Care?
- How long will your loved one remain in Intensive Care?
What does the Respiratory System do ?
The respiratory system consists of the lungs, airways and blood vessels. The respiratory system inhales oxygen into the body and exchanges oxygen by removing carbon dioxide from the body. A normal breath requires a complex coordination between the nervous system (brain & spinal cord) and the muscles of breathing (including the diaphragm and muscles between the ribs).
Abnormal and or inadequate breathing can occur as a result of:
- An interruption to the nervous system (head injuries or spinal injuries for example)
- Barriers to the absorption of oxygen (eg fluid or secretions in the alveoli);
- Obstruction to the flow of gases through the lungs, both breathing in or out (eg asthma);
- Damage to the rib cage such as rib fractures or flail chest(in motor vehicle trauma for example);
- Pneumothorax(deflation of one part of the lung)
- Haemothorax(infiltration with blood to parts of the lung)
- Pain, which makes taking a normal breath difficult.
A number of respiratory conditions can result in respiratory failure and require Intensive Care or High dependency Unit admission. It is often that respiratory failure results in ventilation support (help with breathing). This support may be through the use of oxygen masks, BIPAP or Non- Invasive Ventilation(NIV) or via a Breathing Tube (endotracheal tube) and Ventilators (Breathing Machines)
This image was obtained using a Google image search
Many respiratory conditions, including the above, can lead to admission to Intensive Care or High dependency Care Units. In those units oxygen and/or ventilator support may be initiated ranging from Oxygen Therapy via Oxygen mask to Non- Invasive Ventilation(NIV) or BIPAP ventilation or if the Patient’s condition deteriorates further a Breathing Tube (endotracheal tube) and mechanical ventilation on Ventilators (Breathing Machines) may be required.
This image was obtained using a Google image search
Diagnosis
Pleural effusion is usually diagnosed on the basis of medical history and physical exam, and confirmed by Chest X-ray. Once accumulated fluid is more than 300 ml, there are usually detectable clinical signs in your loved one, such as decreased movement of the chest on the affected side, stony dullness to percussion over the fluid, diminished breath sounds on the affected side, decreased vocal resonance and fremitus(palpable vibration), and pleural friction rub. Above the effusion, where the lung is compressed, there may be bronchial breathing and egophony(increased resonance of voice sounds heard when auscultating the lungs). In large effusion there may be tracheal deviation away from the effusion. A systematic review (2009) published as part of the Rational Clinical Examination Series in the Journal of the American Medical Association (JAMA) showed that dullness to conventional percussion was most accurate for diagnosing pleural effusion.
Other diagnostic tests may include
- CT of the chest
- Ultrasound of the chest
- Pleural fluid analysis
 Massive left sided Pleural Effusion on a chest X-ray
Massive left sided Pleural Effusion on a chest X-ray
This image was found using a google search
Signs& Symptoms in Pleural Effusion
- Shortness of breath
- Chest pain, usually a sharp pain that is worse with cough or deep breaths
- Cough
- Hiccups
- Rapid breathing
- low oxygen saturation
- poor blood gases
- anxiety and distress
- low albumin blood levels
Treatment
Treatment of the pleural effusion depends on the underlying cause and not all pleural effusions will be removed or drained.
Therapeutic aspiration may be sufficient; larger effusions may require insertion of an intercostal drain (either pigtail or surgical). When managing these chest tubes, it is important to make sure the chest tubes do not become occluded or clogged. A clogged chest tube in the setting of continued production of fluid will result in residual fluid left behind when the chest tube is removed. This fluid can lead to complications such as hypoxia due to lung collapse from the fluid, or fibrothorax, later, when the space scars down. Repeated effusions may require chemical (talc, bleomycin, tetracycline/doxycycline), or surgical pleurodesis, in which the two pleural surfaces are scarred to each other so that no fluid can accumulate between them. This is a surgical procedure that involves inserting a chest tube(Under Water Seal Drain & Chest Tube), then either mechanically abrading the pleura or inserting the chemicals to induce a scar. This requires the chest tube to stay in until the fluid drainage stops. This can take days to weeks and can require prolonged hospitalizations. If the chest tube becomes clogged, fluid will be left behind and the pleurodesis will fail.
In thoracentesis the doctor, using a local anaesthetic , carefully inserts a needle through the chest wall into the pleural space and obtains a specimen of fluid. If the collection is large an intercostal drain (chest tube drain and water seal system) may need to be inserted to drain the fluid collection.
What happens in Intensive Care?
Patients are not admitted to Intensive Care with a pleural effusion unless it is quite large and causes a serious deterioration into respiratory dysfunction. However some Patients in Intensive Care may have or develop a pleural effusion from other causes whilst in ICU, such as Post Cardiac Surgery(Coronary Artery Bypass Graft (CABG)) or post Lung Transplantation.
If your loved one requires admission to Critical Care(Intensive Care or High Dependency), he or she requires
- Your loved one will be closely monitored using a Bedside Monitors.
- Initially oxygen and respiratory support might be commenced via na oxygen mask or via Non- Invasive Ventilation(NIV) or BIPAP ventilation
- In Intensive Care your loved one will very likely require a Breathing Tube (endotracheal tube) and mechanical ventilation on Ventilators (Breathing Machines)
- Frequent Chest X-rays and blood tests (Blood& Pathology tests in Intensive Care)especially arterial blood gases (ABGs) will be performed regularly
How long will your loved one remain in Intensive Care?
The length of time in ICU and prognosis will depend on the cause of the pleural effusion and the Patient’s other diagnoses. Once stability is achieved, intensive care length of stay will be minimal.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
Related Articles:
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- How long can a breathing tube or an endotracheal tube can stay in?
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Why does my loved one need a Tracheostomy in Intensive Care?
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- Be more selfish if your loved one is critically ill in Intensive Care
- How to stay positive if your loved one is critically ill in Intensive Care
- 4 ways on how to be more persuasive if your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- How long does it take to wake up from a Traumatic brain injury or severe head injury
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


