What is (Acute) Pancreatitis?
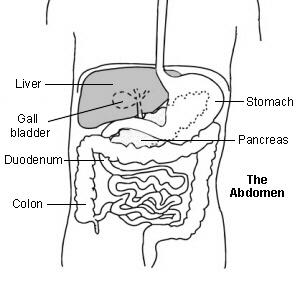
Pancreatitis is the inflammation of the Pancreas which requires immediate medical attention and hospitalization during an attack that has multiple causes and symptoms. It occurs when pancreatic enzymes (especially trypsin) that digest food are activated in the pancreas instead of the small intestine. It may be acute—beginning suddenly and lasting a few days, or chronic—occurring over many years. Acute pancreatitis (inflammation of the Pancreas) comes in mild and severe forms. The main cause of Pancreatitis is gall stones(cholelithiasis) and excess alcohol consumption
The mild form of Pancreatitis usually requires conservative management and therapy with your loved one staying Nil By Mouth(NBM) and therefore not being allowed to eat and drink in order to rest the Pancreas. For severe forms of Pancreatitis where other organs such as the liver, the gall bladder are affected, surgery such as the surgical removal of the gall stones(Cholecystectomy) is required. In the acute phase and if the Pancreatitis is severe admission to Intensive Care may be necessary.
- What does the Pancreas do?
- What is Pancreatitis?
- What Happens in Intensive Care?
- How long will your loved one remain in Intensive Care?
What does the Pancreas do?
The Pancreas is a glandular organ in the digestive system and endocrine system. It is both an endocrine gland producing several important hormones, including insulin and glucagon(maintenance of normal blood sugar), somatostatin, and pancreatic polypeptide, and a digestive organ, secreting pancreatic juice containing digestive enzymes that assist the absorption of nutrients and the digestion in the small intestine. These enzymes help to further break down the carbohydrates, proteins, and lipids in semi digested food.
What happens in Intensive Care?
- Treatment for acute pancreatitis will include intravenous fluids, fasting the Patient
- A urinary catheter is used to monitor urine output and a Nasogastric Tubes will be used to rest the Pancreas and the intestine or if your loved one requires ventilation
- Pain relief may be given using a Patient controlled analgesic device (known as a PCA) or a continuous infusion of Morphine/ Fentanyl or other ‘opiate’ pain relief.
- Your loved one will be fed intravenously with TPN(Total Parenteral Nutrition)
- Your loved one will require monitoring using a Bedside Monitors and an Arterial Catheter(Arterial Line)
- You can expect your loved one to have frequent Chest X-rays and blood tests(Blood& Pathology tests in Intensive Care) especially arterial blood gases (ABGs)
- Initially oxygen and respiratory support might be commenced via an oxygen mask or via Non- Invasive Ventilation(NIV) or BIPAP ventilation
- If your loved one develops respiratory(breathing) difficulties, full ventilation using a Ventilators(Breathing Machine) and a Breathing Tube (endotracheal tube) may be required to improve and maintain the oxygen delivery
- Sedation may be used if your loved one is in an induced coma for ventilator and endotracheal tube tolerance
- Infusion pumps are administering drugs to support your loved ones blood pressure and haemodynamic system, as well as intravenous fluids may be administered via a central venous catheter/ CVC(Central Venous Lines)
- If the acute Pancreatitis is really severe, other complications such as severe shock, Acute lung failure(Adult Respiratory Distress Syndrome (ARDS) and/or Acute Kidney(Renal) Failure may develop

How long will your loved one remain in Intensive care?
Around 20 to 30% of Patients with acute pancreatitis will have severe disease and face a long complicated recovery and some may experience a number of setbacks. This can mean weeks to months in intensive care or repeated admissions to intensive care. A number of Patients will require more than 1 operation to remove dead pancreatic tissue or to drain abscesses. A small number of Patients will develop multiple complications including shock or kidney or respiratory failure. This group of Patients will experience a long and difficult recovery and have an increased risk of death.
A long term stay over weeks or months in Intensive Care may require ongoing mechanical ventilation with Tracheostomy and a sometimes difficult and slow weaning process off the ventilator.
If your loved one faces long-term treatment and long-term ventilation with Tracheostomy in Intensive Care, please visit www.intensivecareathome.com.au for alternative information and alternative treatment options.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual Patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
How can you have PEACE OF MIND, control, power and influence whilst your loved one is critically ill in Intensive Care?
You get to that all important feeling of PEACE OF MIND, CONTROL, POWER AND INFLUENCE when you download your FREE “INSTANT IMPACT” report NOW by entering your email below! In Your FREE “INSTANT IMPACT” report you’ll learn quickly how to get PEACE OF MIND, real power and real control and how you can influence decision making fast, whilst your loved one is critically ill in Intensive Care! Your FREE “INSTANT IMPACT” Report gives you in-depth insight that you must know whilst your loved one is critically ill or is even dying in Intensive Care! Sign up and download your FREE “INSTANT IMPACT” REPORT now by entering your email below!
In your FREE “INSTANT IMPACT” REPORT you’ll learn how to speak the “secret” Intensive Care language so that the doctors and the nurses know straight away that you are an insider and that you know and understand what’s really happening in Intensive Care!
In your FREE reports you’ll also discover
- How to ask the doctors and the nurses the right questions
- Discover the many competing interests in Intensive Care and how your critically ill loved one’s treatment may depend on those competing interests
- How to eliminate fear, frustration, stress, struggle and vulnerability even if your loved one is dying
- 5 “killer” tips& strategies helping you to get on the right path to PEACE OF MIND, control, power and influence in your situation
- You’ll get real world examples that you can easily adapt to your and your critically ill loved one’s situation
- How to stop being intimidated by the Intensive Care team and how you will be seen as equals
- You’ll get crucial ‘BEHIND THE SCENES’ insight so that you know and understand what is really happening in Intensive Care
- How you need to manage doctors and nurses in Intensive Care(it’s not what you think)
Make sure you also check out our “blog” section for tips& strategies and also check out our “your questions answered” section where we answer your questions or send me an email to [email protected] with your questions!
Sincerely, your Friend
Patrik Hutzel
Related Articles:
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- How long does it take to wake up from a Traumatic brain injury or severe head injury?
- What you need to do if your loved one in Intensive Care is brain dead or is considered for organ donation
- What is an induced coma and why is my critically ill loved one in an induced coma?
- How long can a breathing tube or an endotracheal tube can stay in?
- How long should a Patient be on a ventilator before having a Tracheostomy?
- Why does my loved one need a Tracheostomy in Intensive Care?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- Be more selfish if your loved one is critically ill in Intensive Care
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


