What are Oesophageal Varices?
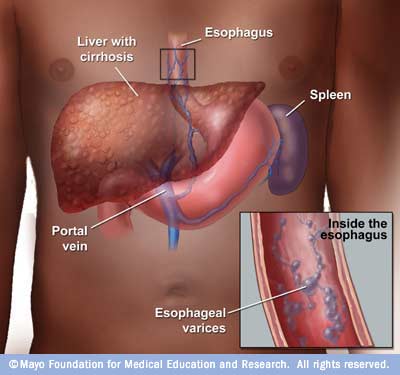
Oesophageal varices are extremely dilated sub-mucosal veins in the lower third of the oesophagus(passage from mouth to stomach). They are most often a consequence of portal hypertension, commonly due to Liver cirrhosis; Patients with Oesophageal varices have a strong tendency to develop bleeding.
Oesophageal varices are diagnosed with endoscopy. Oesophageal Varices resemble varicose veins, but they appear inside the oesophagus and occasionally they occur in the stomach.
Oesophageal Varices develop when the liver develops scar tissue, usually caused by liver cirrhosis (also see Liver Failure). Scar tissue in the liver increases the pressure in the liver and in the veins. The veins leading away from the liver, including the Oesophageal veins, have an increased pressure with the result of the vein walls getting thinner and therefore they are at risk of bursting with the result of a severe bleed. The veins in the oesophagus and in the stomach are the veins that are directly connected to the liver and are directly affected if the liver develops scar tissue.
- Signs and Symptoms
- What Happens in Intensive Care?
- How long will your loved one remain in Intensive Care?
This image found at this Website
Signs and Symptoms
Oesophageal varices usually don’t cause signs and symptoms unless they bleed. Signs and symptoms of bleeding Oesophageal varices include:
- Vomiting blood
- Black, tarry or bloody stools
- Shock, in severe cases
What Happens in Intensive Care?
- your loved one will require monitoring using a Bedside Monitors and an Arterial Catheter(Arterial Line)
- You can expect your loved one to have frequent Chest X-rays and blood tests(Blood& Pathology tests in Intensive Care) especially arterial blood gases (ABGs)
- Initially oxygen and respiratory support might be commenced via an oxygen mask or via Non- Invasive Ventilation(NIV) or BIPAP ventilation
- Full ventilation using a Ventilators(Breathing Machine) and a Breathing Tube (endotracheal tube) will usually be required to improve and maintain the oxygen delivery, especially if your loved one requires Balloon Tamponade Tubes
- Sedation may be used if your loved one is in an induced coma and requires mechanical Ventilation with Ventilators(Breathing Machine)
- Infusion pumps are administering drugs to support your loved ones blood pressure and haemodynamic system, as well as intravenous fluids may be administered via a central venous catheter/ CVC(Central Venous Lines)
- An NG Tube (Nasogastric Tubes) is usually inserted into your loved ones stomach, in order to commence nutrition or to remove fluids
- Urine Output is usually measured hourly, after insertion of a Urinary Catheter
- Medications such as terlipressin or vasopressin may be given to help reduce pressure in the liver.
- It is crucial to find the source of bleeding. This can be doen via Endoscopy(video camera) that can be inserted in the Oesophagus and the source of bleeding can be found. Drugs may be injected to cause the vessels to constrict and stop the bleeding
- If the bleeding is extremely severe, Balloon Tamponade Tubes(balloon tamponade device) may be inserted into the Oesophagus and stomach. Once the balloon is inserted, air pressure is inflated into the balloon in order to put pressure on the bleeding source(s) and stop the bleeding. The balloon tubes may stay in situ for 24-48 hours.
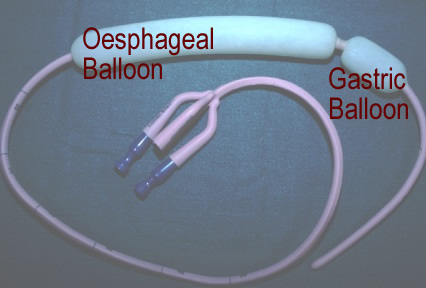
This is an example of a balloon tamponade tube
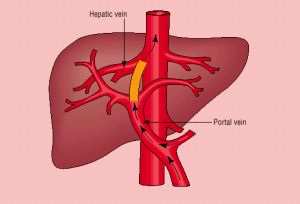
Further surgery may be needed to reduce portal hypertension. This procedure called transjugular intrahepatic portosystemic shunt (TIPPS). A metal opening device is placed in the liver connecting the hepatic and portal veins this allows blood to flow through a different path.
How long will your loved one remain in Intensive Care?
The time spent in Intensive Care will vary from Patient to Patient and can vary from a few days to weeks. How well your loved one recovers depends on a number of factors including severity of liver disease and amount of bleeding.
Are there any complications?
Complications may include continuous bleeding. If liver cirrhosis is the reason for the development of Oesophageal Varices and the bleeding, it is not uncommon for the blood to be very thin, as Liver Cirrhosis or Liver Failure often leads to Coagulopathy, which is a blood clotting and bleeding disorder). Clotting factors are usually chemically synthesised in the liver, however in Patients with Liver cirrhosis or Liver Failure, the liver is unable to synthesise the clotting factors and as a result the Patient is at high risk of bleeding.
Any Questions?
Of course, if you have any questions or concerns, please discuss them with the ICU nurses and doctors.
All Intensive Care interventions and procedures carry a degree of potential risk even when performed by skilled and experienced staff. Please discuss these issues with the medical and nursing staff who are caring for your loved one.
The information contained on this page is general in nature and therefore cannot reflect individual Patient variation. It is meant as a back up to specific information which will be discussed with you by the Doctors and Nurses caring for your loved one. INTENSIVE CARE HOTLINE attests to the accuracy of the information contained here BUT takes no responsibility for how it may apply to an individual Patient. Please refer to the full disclaimer.
Related Articles:
- What is an induced coma and why is my critically ill loved one in an induced coma?
- The 3 most dangerous mistakes that you are making but you are unaware of, if your loved one is a critically ill Patient in Intensive Care
- How to always achieve your goals whilst your loved one is critically ill in Intensive Care
- Why you must make up your own mind about your critically ill loved one’s situation in Intensive Care even if you’re not a doctor or a nurse!
- Follow this proven 5 step process on how to be in control and influential if your loved one is a long-term Patient in Intensive Care
- How to take control if your loved one has a severe brain injury and is critically ill in Intensive Care
- How long does it take to wake up from a Traumatic brain injury or severe head injury?
- What you need to do if your loved one in Intensive Care is brain dead or is considered for organ donation
- What is an induced coma and why is my critically ill loved one in an induced coma?
- How long can a breathing tube or an endotracheal tube can stay in?
- How long should a Patient be on a ventilator before having a Tracheostomy?
- Why does my loved one need a Tracheostomy in Intensive Care?
- How long is a Patient kept on a BIPAP machine in Intensive Care?
- How to quickly take control and have real power and influence if your loved one is critically ill in Intensive Care
- Tracheostomy and weaning off the ventilator in Intensive Care, how long can it take?
- My sister has been in ICU for 21 weeks with Tracheostomy and still ventilated. What do we need to do?
- Severe lung failure and my aunty is not expected to survive…
- Be more selfish if your loved one is critically ill in Intensive Care
- 3 quick steps on how to position and prepare yourself well mentally, whilst your loved one is critically ill in Intensive Care
- How to get what you want whilst your loved one is critically ill in Intensive Care
- 5 steps to become a better negotiator if your loved one is critically ill in Intensive Care
- 5 Ways to have control, power and influence while your loved one is critically ill in Intensive Care
- How to make sure that your values and beliefs are known whilst your loved one is critically ill in Intensive Care
- How to make sure that “what you see is always what you get” whilst your loved one is critically ill in Intensive Care
- What the doctors and the nurses behaviour in Intensive Care is telling you about the culture in a unit
- Family Meetings in Intensive Care or the Elephant in the Room
- What you need to do if your loved one is dying in Intensive Care(part one)
- What you need to do if your loved one is dying in Intensive Care(part two)
- Intensive Care at its best?
- How INTENSIVECAREHOTLINE.COM Can Help You
- What you and your Family need to do if your critically ill loved one is very sick in Intensive Care and faces an uncertain future
- How long can somebody stay in Intensive Care?
- My Family can’t agree on what’s best for my sister in Intensive Care…Help!
- My husband is dying in Intensive Care, but we need more time…
- My mother sustained serious brain damage after a stroke and she now is in multi- organ failure


